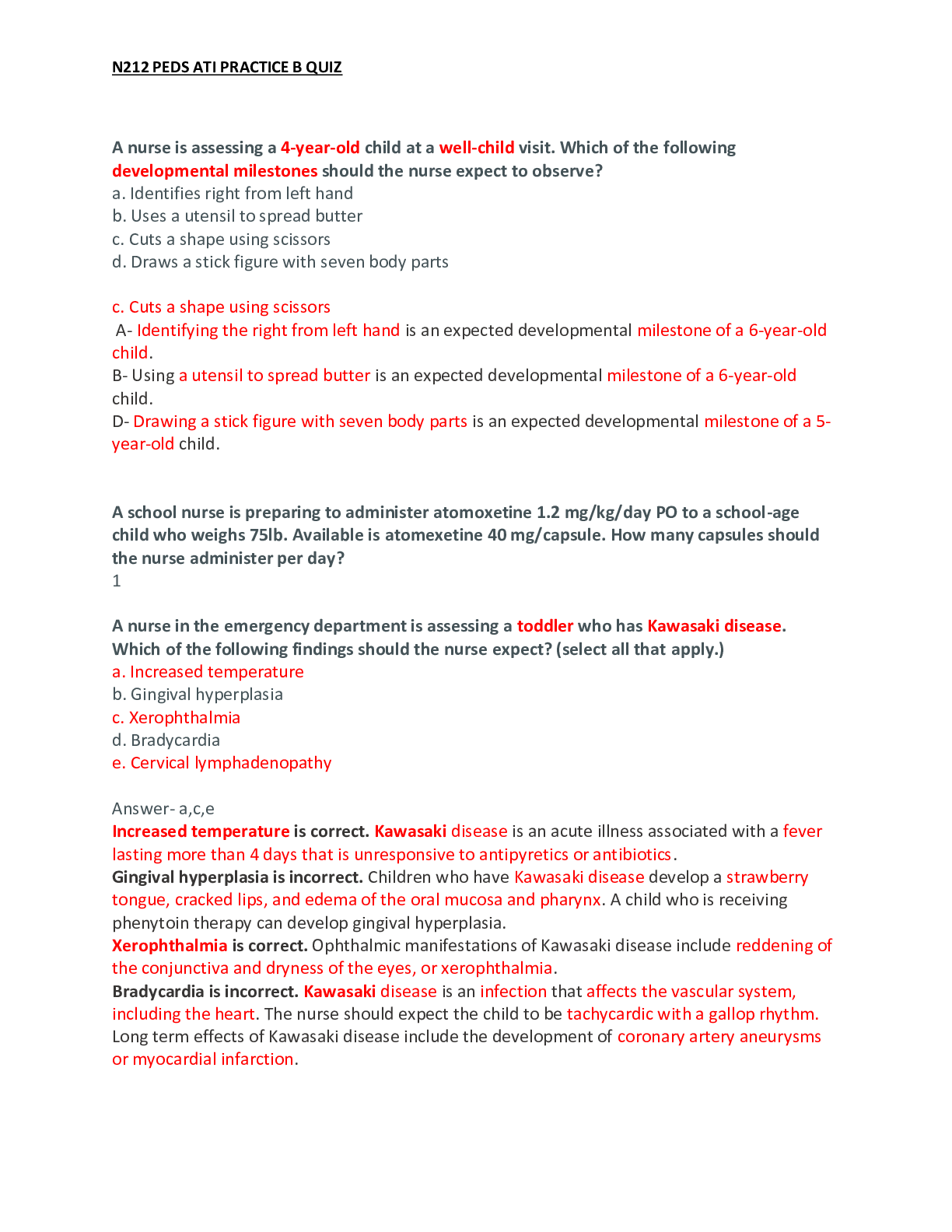
N212 PEDS ATI PRACTICE B QUIZ
A nurse is assessing a 4-year-old child at a well-child visit. Which of the following developmental milestones should the nurse expect to observe?
a. Identifies right from left hand
b. Uses a utensil to spread butter
c. Cuts a shape using scissors
d. Draws a stick figure with seven body parts
c. Cuts a shape using scissors
A- Identifying the right from left hand is an expected developmental milestone of a 6-year-old
child.
B- Using a utensil to spread butter is an expected developmental milestone of a 6-year-old child.
D- Drawing a stick figure with seven body parts is an expected developmental milestone of a 5- year-old child.
A school nurse is preparing to administer atomoxetine 1.2 mg/kg/day PO to a school-age child who weighs 75lb. Available is atomexetine 40 mg/capsule. How many capsules should the nurse administer per day?
1
A nurse in the emergency department is assessing a toddler who has Kawasaki disease. Which of the following findings should the nurse expect? (select all that apply.)
a. Increased temperature
b. Gingival hyperplasia
c. Xerophthalmia
d. Bradycardia
e. Cervical lymphadenopathy
Answer- a,c,e
Increased temperature is correct. Kawasaki disease is an acute illness associated with a fever
lasting more than 4 days that is unresponsive to antipyretics or antibiotics.
Gingival hyperplasia is incorrect. Children who have Kawasaki disease develop a strawberry tongue, cracked lips, and edema of the oral mucosa and pharynx. A child who is receiving phenytoin therapy can develop gingival hyperplasia.
Xerophthalmia is correct. Ophthalmic manifestations of Kawasaki disease include reddening of the conjunctiva and dryness of the eyes, or xerophthalmia.
Bradycardia is incorrect. Kawasaki disease is an infection that affects the vascular system, including the heart. The nurse should expect the child to be tachycardic with a gallop rhythm. Long term effects of Kawasaki disease include the development of coronary artery aneurysms or myocardial infarction.
N212 PEDS ATI PRACTICE B QUIZ
Cervical lymphadenopathy is correct. The child who has Kawasaki disease may develop enlarged cervical nodes on one side of the neck that are nontender and greater than 1.5 cm in size.
A nurse is teaching a school-age child who has a new diagnosis of type 1 diabetes MELITIS. The nurse should identify which of the following statements by the child as understanding the teaching?
a. I will puncture the pad of my finger when I am testing my blood glucose."
b. "I will give myself a shot of regular insulin 30 minutes before I eat breakfast." c. "I will eat a snack of 5 grams of carbohydrates if my blood glucose is low."
d. "I will decrease the amount of fluids I drink when I am sick."
Answer- b. "I will give myself a shot of regular insulin 30 minutes before I eat breakfast." The child should administer regular insulin 30 min before meals so that the onset coincides with
food intake.
A- The child should avoid puncturing the pads of the fingers because they have fewer blood vessels and more nerve fibers. Instead, the child should puncture the skin to either side of the finger pad to promote blood flow and decrease pain.
C- The child should eat a snack of 15 g of carbohydrates, such as 120 mL (4 oz) of fruit juice or 66 g (1/2 cup) of ice cream, to rapidly increase a mild hypoglycemic reaction.
D- During acute illness the child is prone to hyperglycemia and ketonuria and is at risk for dehydration. Therefore, the child's fluid intake should increase rather than decrease.
A school nurse is assessing an adolescent who has scoliosis. Which of the following findings should the nurse expect?
a. Increase in anterior convexity of the lumbar spine
b. Increased curvature of the thoracic spine
c. Lateral flexion of the neck
d. A unilateral rib hump
Answer- d. A unilateral rib hump
When assessing an adolescent for scoliosis, the school nurse should expect to see a unilateral rib hump with hip flexion. This results from a lateral S- or C-shaped curvature to the thoracic spine resulting in asymmetry of the ribs, shoulders, hips, or pelvis. Scoliosis can be the result of a neuromuscular or connective tissue disorder, or it can be congenital in nature.
A- An increased anterior convexity of the lumbar spine is a manifestation of lordosis. An expected finding in toddlers, lordosis can indicate a complication of a disease process, such as flexion contractures, congenital dislocation of the hip, or obesity, when seen in older children. B- An increased curvature of the thoracic spine is a manifestation of kyphosis. Kyphosis can be a manifestation of a congenital condition or disease process such as rickets, or it can be posture-
related. In posture-related kyphosis, the adolescent presents with rounded shoulders and a slouching posture.
N212 PEDS ATI PRACTICE B QUIZ
C- Lateral flexion of the neck is an indication of torticollis as a result of contracture of the sternocleidomastoid muscle. Torticollis can be congenital, the result of intrauterine fetal posturing or abnormality of the cervical spine, or it can be acquired, due to such factors as a
traumatic lesion to the sternocleidomastoid muscle.
A nurse is reviewing the lumbar puncture results of a school-age child suspected of having bacterial meningitis. Which of the following results should the nurse identify as a finding associated with bacterial meningitis?
a. Decreased cerebrospinal fluid pressure
b. Decreased WBC count
c. Increased protein concentration d. Increased glucose level
Answer- c. Increased protein concentration. The nurse should recognize that an increased protein concentration in the spinal fluid is a finding associated with bacterial meningitis.
A- Increased cerebrospinal fluid pressure is a finding associated with bacterial meningitis.
B- An increased WBC count in the spinal fluid is a finding associated with bacterial meningitis. D- A decreased glucose level in the spinal fluid is a finding associated with bacterial meningitis.
A nurse is planning care for a preschooler who has cystic fibrosis. Which of the following interventions should the nurse include in the plan?
a. Administer pancreatic enzymes 2 hr after meals.
b. Decrease pancreatic enzymes if steatorrhea develops.
c. Limit fluid intake to 750 mL per day.
d. Increase fat content in the child's diet to 40% of total calories.
Answer - d. Increase fat content in the child's diet to 40% of total calories. A child who has cystic fibrosis is unable to properly digest fats due to fibrosis of the pancreas and limited secretion of pancreatic enzymes. The nurse should increase the child's fat intake to equal 40% of total caloric intake.
A- The nurse should plan to administer pancreatic enzymes within 30 min of meals and snacks.
B- A child who has cystic fibrosis and develops steatorrhea, or fatty stools, needs to increase the intake of pancreatic enzymes.
C- The nurse should encourage fluid intake, rather than restrict it, to prevent dehydration caused by the loss of sodium and chloride through perspiration.
A nurse is assessing a toddler who has gastroenteritis and is exhibiting manifestations of dehydration. Which of the following findings should the nurse address first?
a. Skin breakdown
b. Hypotension
c. Hyperpyrexia
d. Tachypnea
N212 PEDS ATI PRACTICE B QUIZ
Answer- d. Tachypnea. When using the airway, breathing, circulation approach to client care, the first finding the nurse should address is the toddler's tachypnea, which results when the kidneys are unable to excrete hydrogen ions and produce bicarbonate leading to metabolic
acidosis.
A- Toddlers who have gastroenteritis and are dehydrated are at increased risk for skin breakdown because of changes in circulation and loss of skin elasticity. However, the nurse should address another finding first.
B- Toddlers who have gastroenteritis and are dehydrated may exhibit hypotension because of reduced blood volume. However, the nurse should address another finding first.
C- Toddlers who have gastroenteritis and are dehydrated may exhibit hyperpyrexia, or fever, which is caused by the effect of fluid volume depletion on the hypothalamus. However, the nurse should address another finding first.
A nurse is discussing organ donation with the parents of a school-age child who has sustained brain death due to a bicycling accident. Which of the following actions should the nurse take
first?
a. Inform the parents that written consent is required prior to organ donation. b. Provide written information to the parents about organ donation.
c. Ask the provider to explain misconceptions of organ donation to the parents. d. Explore the parents' feelings and wishes regarding organ donation.
Answer- d. Explore the parents' feelings and wishes regarding organ donation. The first action the nurse should take when using the nursing process is assessment. Exploring the parents' feelings and wishes regarding organ donation will assist the nurse in determining if organ donation is appropriate for this family and should be done prior to taking other actions.
A- The nurse should inform the parents that written consent is required prior to organ donation to document that the parents have consented to organ donation and that the provider has addressed any questions or concerns the parents may have. However, there is another action that the nurse should take first.
B- The nurse should provide written information to the parents to enhance their understanding about organ donation. However, there is another action that the nurse should take first.
C- The nurse should ask the provider to explain misconceptions of organ donation to the
parents, because it is important that they have accurate information before making a final decision. However, there is another action that the nurse should take first.
A nurse in an emergency department is caring for a school-age child who has appendicitis and rates his abdominal pain 7 on a 0 to 10 scale. Which of the following actions should the nurse take?
a. Instill a 500 mL tap water enema.
b. Give morphine 0.05mg/kg IV.
c. Administer polyethylene glycol 1g/kg PO.
d. Apply a heating pad to the child's abdomen.
Answer- b. Give morphine 0.05mg/kg IV. A pain level of 7 on a 0 to 10 scale is considered severe and the nurse should administer an analgesic medication for pain relief.
N212 PEDS ATI PRACTICE B QUIZ
A- Administering an enema accelerates bowel motility and increases the risk for perforation of the appendix.
C- Administering laxatives accelerates bowel motility and increases the risk for perforation of
the appendix.
D- Applying heat to the child's abdomen increases the risk for perforation of the appendix.
A nurse is monitoring the oxygen saturation level of an infant using pulse oximetry. The nurse should secure the sensor to which of the following areas on the infant?
a. Wrist
b. Great toe
c. Index finger
d. Heel
Answer - b. Great toe. The nurse should secure the sensor to the great toe of the infant and then place a snug-fitting sock on the foot to hold the sensor in place. The nurse should also
check the skin under the sensor site frequently for pulses, temperature, and color.
A- It is important for the sensor to be positioned in the correct area in order to obtain an accurate reading. The nurse should avoid placing the sensor on the wrist because this placement will result in an inaccurate reading.
C- The nurse should secure the sensor to the index finger of an older child and then use a self- adhering bandage to hold the sensor in place.
D- It is important for the sensor to be positioned in the correct area in order to obtain an accurate reading. The nurse should avoid placing the sensor on the heel of the infant's foot because this placement will result in an inaccurate reading.
A nurse is assessing a school-age child who has an infratentorial brain tumor. Which of the following findings should the nurse identify as a manifestation of increased intracranial pressure?
a. Hypotension
b. Hyperactivity
c. Decreased attention span d. Tachycardia
Answer- c. Decreased attention span. The nurse should recognize decreased attention span, inability to follow commands, and difficulty in school are manifestations of increased intracranial pressure because of the decreased blood flow within the brain.
A- Hypertension is a late manifestation of increased intracranial pressure.
B- Lethargy and decreased activity are manifestations of increased intracranial pressure. D- Bradycardia is a late manifestation of increased intracranial pressure.
A school nurse is assessing a school-age child who has erythema infectious (fifth disease). Which of the following findings should the nurse expect?
a. Koplik spots b. Hoarseness
N212 PEDS ATI PRACTICE B QUIZ
c. Facial rash
d. Splenomegaly
Answer - c. Facial rash. Erythema on the face, predominantly on the child's cheeks, is a manifestation of erythema infectiosum (fifth disease). The erythema causes the child to have the appearance of a "slapped face." The rash lasts from 1 to 4 days.
A- Koplik spots are a manifestation of ).
B- Hoarseness is a manifestation of .
d- Splenomegaly is a manifestation of infectious mononucleosis.
A nurse is reviewing laboratory results of a school-age child who is 1 week postoperative following an open fracture repair. Which of the following values should the nurse identify as an indication of a potential complication?
a. Erythrocyte sedimentation rate 18 mm/hr
b. WBC 6,200/mm3
measles (rubeola
diphtheria
c. C-reactive protein 1.4 mg/L d. RBC 4.7 106/μL
Answer- a. Erythrocyte sedimentation rate 18 mm/hr. An erythrocyte sedimentation rate of 18 mm/hr is above the expected reference range and is an indication of osteomyelitis.
B- A WBC count of 6,200/mm3 is within the expected reference range. An elevated WBC count indicates infection.
C- A C-reactive protein level of 1.4 mg/L is within the expected reference range. An elevated C- reactive protein level is an indication of osteomyelitis.
D- A RBC count of 4.7 106/μL is within the expected reference range. A decreased RBC count indicates hemorrhage.
A nurse is teaching a group of parents about infectious mononucleosis. which of the following statements by a parent should the nurse identify as understanding the teaching?
a. "Mononucleosis is caused by an infection with the Epstein-Barr virus."
b. "Mononucleosis is a bacterial infection requiring 14 days of antibiotics."
c. "A Monospot is a throat culture used to diagnosis mononucleosis."
d. "Children who get mononucleosis will need to refrain from sports for 6 months."
Answer- a. "Mononucleosis is caused by an infection with the Epstein-Barr virus."
Mononucleosis is a mildly contagious illness that occurs sporadically or in groups and is primarily caused by the Epstein-Barr virus.
B- Infectious mononucleosis is caused by the Epstein-Barr virus. No known specific treatment is available for mononucleosis.
C- A Monospot is a blood test that uses a special piece of paper to assist in diagnosing mononucleosis,
N212 PEDS ATI PRACTICE B QUIZ
D- Acute symptoms last approximately 10 days with fatigue lasting up to 4 weeks. Children who have mononucleosis and develop splenomegaly will need to restrict activities for 2 to 3 months to avoid rupturing the spleen.
A hospice nurse is caring for a preschooler who has a terminal illness. The father tells the nurse that he cannot cope anymore and has decided to move out of the house. Which of the following statements should the nurse make?
a. "I think it is important that you provide emotional support for your family at this time."
b. "I agree that you have to do what you feel is best for yourself during this stressful time."
c. "You can't mean that; I'm sure you want to be there for your family."
d. "Let's talk about some of the ways you have handled previous stressors in your life."
Answer- d. "Let's talk about some of the ways you have handled previous stressors in your life." This statement offers a general lead to allow the father to express his feelings and previous actions when faced with stressful situations, as well as help him to focus on ways that he can
cope with the current situation.
A- This statement presents the nurse's opinion and tells the father how he should behave, which can make him feel as if he has to behave as the nurse does and can lead to dependence. B- This statement offers agreement with the father, which implies that the nurse is giving approval.
C- This statement challenges the father by disregarding his feelings, which can make him defensive and resistant to communicating in the future.
A nurse is an emergency department suspects that a toddler has epiglottis. Which of the following actions should the nurse take?
a. Obtain a culture from the toddler's throat.
b. Prepare the toddler for nasotracheal intubation.
c. Visually inspect the epiglottis using a tongue depressor.
d. Administer the Haemophilus influenzae type B conjugate vaccine.
Answer- b. Prepare the toddler for nasotracheal intubation. When is suspected the nurse should prepare for nasotracheal intubation or a tracheostomy, which might be required if the toddler begins to experience severe respiratory distress.
A- When epiglottitis is suspected the nurse should avoid any actions, such as obtaining a throat culture, which can cause further inflammation, irritation, or obstruction of the airway.
C- When epiglottitis is suspected the nurse should avoid any actions, such as direct visualization of the epiglottis with a tongue depressor, which can cause further inflammation, irritation, or obstruction of the airway.
D- The nurse should recommend administration of the Haemophilus influenzae type B conjugate vaccine for infants as a prevention of epiglottitis. The immunization is not used in the
epiglottitis
treatment of acute epiglottitis.
N212 PEDS ATI PRACTICE B QUIZ
A nurse is caring for a toddler who has acute otitis media and a temperature of 40 C (104 F). After administering acetaminophen, which of the following actions should the nurse plan to
take to reduce the toddler's temperature?
a. Apply a cooling blanket to the toddler.
b. Dress the toddler in minimal clothing.
c. Give the toddler a tepid bath.
d. Administer diphenhydramine to the toddler.
Answer- b. Dress the toddler in minimal clothing. The nurse should recognize that dressing the toddler in minimal clothing will expose the skin to air and maximize heat evaporation from the skin, thus reducing the toddler's temperature.
A- Applying a cooling blanket can cause shivering and discomfort, which increases metabolic requirements and is not effective in reducing the toddler's temperature.
C- A tepid bath is lukewarm, which can cause discomfort to the toddler, and is not effective in
reducing fever.
D- Diphenhydramine is an antipruritic rather than an antipyretic medication.
A nurse is assessing an infant who has a ventricular septal defect. Which of the following findings should the nurse expect?
a. Loud, harsh murmur
b. Dysrhythmias
c. Weak femoral pulses d. High blood pressure
Answer- a. Loud, harsh murmur. The nurse should expect to hear a loud, harsh murmur with a ventricular septal defect due to the left-to-right shunting of blood, which contributes to hypertrophy of the infant's heart muscle.
B- Ventricular septal defect does not affect the electrical conduction of the heart. Therefore, the nurse should not expect to hear dysrhythmias when assessing this infant.
C- Weak femoral pulses are a manifestation of coarctation of the aorta.
D- Elevated blood pressure is a manifestation of coarctation of the aorta.
A nurse is providing discharge teaching to the parent of a school-age child who has undergone a tonsillectomy. Which of the following statements by the parent should the nurse identify as understanding the teaching?
a. "My child may resume usual activities since this was just an outpatient surgery."
b. "My child will be able to drink the chocolate milkshake I promised to get for her tonight."
c. "I will notify the doctor if I notice that my child is swallowing frequently."
d. "I will have my child gargle with warm salt water to relieve her sore throat."
N212 PEDS ATI PRACTICE B QUIZ
Answer- c. "I will notify the doctor if I notice that my child is swallowing frequently." The nurse should instruct the parent that frequent swallowing is a sign of bleeding and, if it is observed, to notify the primary care provider immediately.
A- Activity should be limited for up to 10 days to decrease the risk of hemorrhage.
B- Milk products should be avoided because they coat the child's throat, which can initiate a cough response and increase the risk of bleeding. Brown and red foods should be avoided during the immediate postoperative period so that food and fresh or old blood are distinguishable in the child's emesis.
D- Salt water is likely to cause irritation and discomfort and can increase the risk of bleeding following a tonsillectomy. The child should receive adequate pain medication after the procedure and can wear an ice collar if tolerated.
A nurse is assessing an 8-year-old child who has early indications of shock. After establishing an airway and stabilizing the child's respirations, which of the following actions should the
nurse take next?
a. Insert an indwelling urinary catheter. b. Measure weight and height.
c. Initiate IV access.
d. Maintain ECG monitoring.
Answer- c. Initiate IV access. Since the child's airway is established and respirations are stabilized, the next action the nurse should take using the airway, breathing, circulation approach to client care is to establish IV access to maintain the child's circulatory volume.
A- The nurse should insert an indwelling urinary catheter for a child who has early signs of shock. Strict intake and output monitoring is needed because urinary output decreases in shock due to reduced blood flow to kidneys as the body attempts to conserve body fluids. However, there is another action that the nurse should take first.
B- The nurse should measure weight and height of a child who has early signs of shock in order to calculate weight-based drug dosages. However, there is another action that the nurse should take first.
D- The nurse should maintain ECG monitoring for a child who has early signs of shock to
continually assess for changes in cardiac status. However, there is another action that the nurse should take first.
A nurse is admitting a school-age child who has pertussis. Which of the following actions should the nurse take?
a. Place the child in a room with positive-pressure airflow.
b. Place the child in a room with negative-pressure airflow.
c. Initiate contact precautions for the child.
d. Initiate droplet precautions for the child.
Answer- d. Initiate droplet precautions for the child. The nurse should initiate droplet precautions for a child who has , also known as . Pertussis is
pertussis
whooping cough
N212 PEDS ATI PRACTICE B QUIZ
transmitted through contact with infected large-droplet nuclei that are suspended in the air when the child coughs, sneezes, or talks.
A- The nurse should place a child who has undergone an allogeneic hematopoietic stem cell
transplant in a room with positive-pressure airflow to reduce the risk of disease transmission to the child.
B- The nurse should place a child who has an airborne infection, such as measles or varicella, into a room with negative-pressure airflow.
C- The nurse should initiate contact precautions for a child who has an illness that can be transmitted by direct contact or contact with the child's items, such as hepatitis A and rotavirus.
A nurse is caring for a 2-week-old infant who is breastfeeding and requires a heel stick. Which of the following actions should the nurse take to minimize the infant's pain?
a. Instruct the mother not to breastfeed for 1 hr after the procedure.
b. Undress the infant and place him under a radiant warmer prior to the procedure.
c. Administer sucrose to the infant prior to the procedure.
d. Recommend the mother avoid placing the infant in the kangaroo hold after the procedure.
Answer- c. Administer sucrose to the infant prior to the procedure. The nurse should administer sucrose to the infant prior to the procedure. Evidence-based practice indicates that sucrose, as well as non-nutritive sucking with a pacifier, can provide non-pharmacological pain management in infants.
A- Breastfeeding during and immediately following a painful procedure can minimize the infant's pain. Evidence- based practice indicates that infants who were breastfed during the administration of heel sticks and vaccines had less procedure-related pain than those who were swaddled or offered a pacifier.
B- The nurse should use swaddling or other tucking interventions as a non-pharmacological method of providing comfort to the infant, rather than placing him under the radiant warmer. D- The nurse should encourage, rather than discourage, the mother to provide skin-to-skin contact, or kangaroo care, to the infant both during and following the heel stick.
A nurse is teaching a school-age child and his parent about postoperative care following
cardiac catheterization. Which of the following instructions should the nurse include? a. "Stay home from school for 1 week following the procedure."
b. "Follow a diet that is low in fiber for 1 week."
c. "Wait 3 days before taking a tub bath."
d. "Apply a pressure dressing to the site for 3 days."
Answer- c. "Wait 3 days before taking a tub bath." The child should keep the site clean and dry for at least 3 days to reduce the risk of infection. He should not take a tub bath for 3 days to avoid immersion of the incision in water.
A- The child can attend school the next day but he should avoid strenuous activities to prevent bleeding at the insertion site.
B- The child can resume his regular diet after the procedure.
N212 PEDS ATI PRACTICE B QUIZ
D- The parent can remove the pressure dressing the day after the procedure and should apply a new adhesive bandage strip daily to the site for at least the next 2 days.
A charge nurse is preparing to make a room assignment for a newly admitted school-age child. Which of the following considerations is the nurse's priority when making a room assignment?
a. Length of stay
b. Treatment schedule
c. Disease process
d. Self-care ability
Answer- c. Disease process. The transmission of infectious diseases is the greatest risk to this child and other children on the unit; therefore, the child's disease process is the nurse's priority consideration.
A- It is important for the nurse to consider the child's anticipated length of stay because some client rooms may be larger and thus more comfortable for families during long hospitalizations; however, this is not the nurse's priority consideration.
B- It is important for the nurse to consider the child's treatment schedule when making room assignments because children requiring frequent monitoring and treatments should be assigned a room close to the nurses' station if possible; however, this is not the nurse's priority consideration.
D- It is important for the nurse to consider the child's self-care ability when making room assignments because children who require more assistance from nurses or assistive personnel should be assigned a room close to the nurses' station if possible; however, this is not the nurse's priority consideration.
A nurse is assessing a toddler who has leukemia and is receiving his first round of chemotherapy. Which of the following findings is the priority for the nurse to report to the provider?
a. Urticaria
b. Fatigue
c. Vomiting d. Anorexia
Answer- a. Urticaria. The greatest risk to a toddler who is receiving his first round of chemotherapy is an anaphylactic reaction; therefore, urticaria is the priority finding for the nurse to report to the provider. The nurse should monitor the child for anaphylaxis during and up to 1 hr after the infusion is complete, and immediately report associated findings, such as urticaria, rash, angioedema, and wheezing to the provider.
B- Fatigue may be a manifestation of the disease process, an adverse effect of medication, or an indication of infection due to anemia and myelosuppression in the child who is receiving
chemotherapy; however, another finding is the nurse's priority.
N212 PEDS ATI PRACTICE B QUIZ
C- Vomiting may be a manifestation of the disease process, or an adverse effect of medication in the child who is receiving chemotherapy, and although the nurse should administer an antiemetic to the child, another finding is the priority.
D- Anorexia may be a manifestation of the disease process, or an adverse effect of medication in the child who is receiving chemotherapy. Although the nurse should implement measures to encourage intake and continue to monitor nutritional status, another finding is the priority.
A nurse is providing anticipatory guidance to the parents of a 2-week-old infant about risk factors for sudden infant death syndrome (SIDS). Which of the following risk factors should the nurse include in the teaching?
a. Covering the sleeping infant with a blanket
b. Supine sleeping
c. Maternal history of milk allergy d. Pacifier use during sleep
Answer- a. Covering the sleeping infant with a blanket. The use of quilts or blankets to cover the sleeping infant increases the risk of SIDS due to the potential for suffocation. The nurse should recommend the parents dress the infant warmly and increase the temperature in the home.
B - Evidence-based practice indicates that supine sleeping is a protective factor against SIDS. Infants who sleep prone are at risk for SIDS due to the potential for oropharyngeal obstruction, ineffective thermal balance, decreased arousal state, and rebreathing of carbon dioxide.
C - A milk allergy, either the mother's or the infant's, is not a risk factor for SIDS.
D- Evidence-based practice indicates that pacifier use is a protective factor against SIDS. Infants should use a pacifier at naptime and bedtime. Parents whose infants are breastfeeding should wait to have the infant use a pacifier until she is breastfeeding successfully.
A nurse is caring for a school-age child who has experienced a tonic-clonic seizure. Which of the following actions should the nurse take during the immediate postictal period?
a. Place the child in a lateral position.
b. Delay documentation until the child is fully alert. c. Give the child a high-carbohydrate snack.
d. Administer an oral sedative to the child.
Answer- a. Place the child in a lateral position. The nurse should place the child in a lateral position to prevent aspiration.
B- To ensure accurate description of the event, the nurse should document the treatment of the seizure and the postictal period as early as possible.
C- The child should not be given any foods or liquids until protective reflexes have returned to prevent aspiration.
D- The child should not be given anything by mouth until protective reflexes have returned. Any medications needed should be administered via IV or rectal routes.
N212 PEDS ATI PRACTICE B QUIZ
A nurse is caring for an infant who is receiving IV fluids for the treatment of
Tetralogy of
Fallot and begins to have a hyper cyanotic spell. Which of the following actions should the nurse take?
a. Place the infant in a knee-chest position.
b. Administer a dose of meperidine IV.
c. Discontinue administration of IV fluids.
d. Apply oxygen at 2 L/min via nasal cannula.
Answer- a. Place the infant in a knee-chest position. The nurse should place the infant in a knee-chest position during a hypercyanotic spell to decrease the return of desaturated venous blood from the legs and to direct more blood into the pulmonary artery by increasing systemic vascular resistance.
B- The nurse should administer morphine IV to the infant, instead of meperidine, to decrease
infundibular spasms that cause a decrease in pulmonary blood flow and right-to-left shunting. C- The nurse should continue the administration of IV fluids during a hypercyanotic spell to decrease the viscosity of the infant's blood which decreases the risk of a cerebrovascular accident.
D- The nurse should apply oxygen at 100% via face mask to assist with dilation of the pulmonary artery and improve oxygen supply to the brain.
A nurse is planning an educational program for school-age children and their parents about bicycle safety. Which of the following information should the nurse plan to include?
a. The child should be able to stand on the balls of her feet when sitting on the bike.
b. The child should ride her bike 2 feet to the side of other bike riders.
c. The child should wear dark-colored clothing with a fluorescent stripe when riding at night. d. The child should ride the bike facing traffic when it is necessary to ride in the street.
Answer- a. The child should be able to stand on the balls of her feet when sitting on the bike. To decrease the risk for injury, parents should ensure that the bike is the correct size for the child.
When seated on the bike, the child should be able to stand with the ball of each foot touching the ground and should be able to stand with each foot flat on the ground when straddling the bike's center bar.
B- To decrease the risk for injury, children should ride their bikes single file rather than side by side.
C- To decrease the risk for injury when riding a bike at night, children should wear light-colored clothing that has fluorescent material attached. This measure along with fluorescent material on the bike itself makes bike riders more visible to motor vehicle drivers and other bike riders. D- To decrease the risk for injury, bike riders should ride in the direction of the flow of traffic.
N212 PEDS ATI PRACTICE B QUIZ
A nurse is providing anticipatory guidance to the parents of an 8-month-old infant during a well-child visit. Which of the following statements should the nurse make?
a. "Your baby should be able to stand while holding on to furniture."
b. "Your baby should be able to say one to two words."
c. "Your baby should be able to sit unsupported."
d. "Your baby should be able roll a ball to you."
Answer- c. "Your baby should be able to sit unsupported." The nurse should recognize that an infant should sit unsupported at the age of 8 months.
A- The infant should stand while holding on to furniture at the age of 10 months.
B- The infant should say one word at the age of 10 months.
D- The infant should roll a ball to another person at the age of 11 months.
A nurse is providing teaching to the parent of an infant who has diaper dermatitis. The nurse
should teach the parent to apply which of the following to the affected area?
a. Zinc oxide
b. Antibiotic ointment c. Talcum powder
d. Antiseptic solution
Answer- a. Zinc oxide. Diaper dermatitis is a common inflammatory skin disorder caused by contact with an irritant such as urine, feces, soap, or friction, and takes the form of scaling, blisters, or papules with erythema. Providing a protective barrier, such as zinc oxide, against the irritants allows the skin to heal.
B- Diaper dermatitis can be the result of an overgrowth of yeast, such as Candida albicans, on the skin. Treatment for yeast-related dermatitis includes a topical antifungal medication; however, antibiotic ointment is not recommended for the treatment of diaper dermatitis.
C- Diaper dermatitis can be treated with several different products at the same time, including a protective ointment and a protective powder such as a powder made with karaya or cornstarch; however, talcum powder is not recommended for the treatment of diaper dermatitis because this has been linked to respiratory disorders in infants.
D- Infants who have diaper dermatitis should have the affected areas gently washed with water and a mild soap. Antiseptic solution is not recommended because this can cause burning and pain to the infant.
A nurse is interviewing the parent of an 18-month-old toddler during a well-child visit. The nurse should identify that which of the following findings indicates a need to assess the toddler for hearing loss?
a. The toddler has a vocabulary of 25 words.
b. The toddler developed a mild rash following a recent varicella vaccine.
c. The toddler's Moro reflex is absent.
d. The toddler received tobramycin during a hospitalization 2 weeks ago.
N212 PEDS ATI PRACTICE B QUIZ
Answer- d. The toddler received tobramycin during a hospitalization 2 weeks ago. The nurse should identify tobramycin as an aminoglycoside, which is an ototoxic medication that can
cause mild to moderate hearing loss, and should assess the toddler for a hearing impairment. A- At the age of 18 months the toddler should have a vocabulary of at least 10 words; therefore, a vocabulary of 25 words does not indicate a need to assess the toddler for hearing loss.
B- Approximately 1 in 25 people develop a mild rash following administration of the varicella vaccine. This reaction does not indicate a need to assess the toddler for hearing loss.
C- Primitive reflexes, such as Moro, rooting, and tonic neck, disappear by 5 months of age; therefore, an absent Moro reflex does not indicate a need to assess the toddler for hearing loss.
A nurse is preparing to suction an infant who has a tracheostomy. Which of the following actions should the nurse take?
a. Routinely suction every 30 min.
b. Instill 0.9% sodium chloride prior to suctioning. c. Limit suctioning pressure to 40 mm Hg.
d. Suction for 5 seconds or less.
Answer- d. Suction for 5 seconds of less. The nurse should suction an infant who has a tracheostomy for 5 seconds or less to prevent hypoxia.
A- The nurse should only suction an infant who has a tracheostomy as often as needed to prevent hypoxia and to maintain patency of the tube.
B- The practice of instilling normal saline before suctioning a child who has a tracheostomy is not supported by research and is not a recommended practice because it causes a decrease in oxygen saturation that can last up to 2 min following suctioning.
C- The nurse should ensure the vacuum pressure is set between 60 and 100 mm Hg for an infant. A pressure of 40 mm Hg could be insufficient to effectively clear the infant's airway.
A nurse is teaching the mother of a 6-month-old infant about . Which of the
teething
following statements should the nurse make?
a. "Your baby may pull at her ears when she is teething."
b. "Rub your baby's gums with an aspirin to decrease her discomfort." c. "Place a beaded teething necklace around your baby's neck."
d. "Your baby's upper middle teeth will erupt first."
Answer- a. "Your baby may pull at her ears when she is teething." The nurse should inform the mother that teething can result in discomfort for the infant. Therefore, the mother should look for indications such as pulling on the ears, difficulty sleeping, increased drooling, or increased fussiness.
N212 PEDS ATI PRACTICE B QUIZ
B- The parent should avoid using aspirin or teething powders due to the risk of aspiration, infection, or irritation of the gum tissues. The nurse should recommend cold teething rings or gently rubbing the infant's gums with a cold cloth to minimize discomfort.
C- Necklaces can result in suffocation and choking. Therefore, the nurse should instruct the mother to avoid placing these on the infant.
D- The nurse should inform the mother that the eruption of an infant's teeth begins with the lower central incisors.
A nurse is caring for an adolescent who received a kidney transplant. Which of the following findings should the nurse identify as an indication the adolescent is rejecting the kidney?
a. Negative leukocyte esterase
b. Serum creatinine 3.0 mg/dl
c. Negative urine protein d. Urine output 40 ml/hr
Answer- b. Serum creatinine 3.0 mg/dl. Creatinine is a byproduct of protein metabolism and is excreted from the body through the kidneys. An elevated serum creatinine level, therefore, can be an indication that the kidneys are not functioning. The nurse should identify that the adolescent's serum creatinine level is higher than the normal reference range and may indicate rejection of the kidney.
A- Negative leukocyte esterase level is an expected finding and indicates that the adolescent does not have a urinary tract infection. Leukocyte esterase does not provide information about rejection of the kidney.
C- Negative urine protein is an expected finding and does not indicate rejection of the kidney. D- Oliguria is less than 20 ml/hr of urine and is a sign of kidney rejection. This urine output amount does not indicate rejection of the kidney.
A nurse is caring for a school-age child who is receiving a blood transfusion. Which of the following manifestations should alert the nurse to a possible hemolytic transfusion reaction? a. Laryngeal edema
b. Flank pain
c. Distended neck veins d. Muscular weakness
Answer- b. Flank pain. The nurse should recognize that flank pain is caused by the breakdown of RBCs and is an indication of a hemolytic reaction to the blood transfusion.
A- Laryngeal edema is an indication of an allergic reaction to the blood transfusion.
C- Distended neck veins are an indication of circulatory overload, which is a complication of a blood transfusion.
D- Muscle weakness is an indication of an electrolyte disturbance, which is a complication of a blood transfusion.
N212 PEDS ATI PRACTICE B QUIZ
A community health nurse is assessing an 18-month-old toddler in a community day care. Which of the following findings should the nurse identify as a potential indication of physical
?
neglect
a. Resists having an axillary temperature taken
b. Exhibits withdrawal behaviors when her parent leaves c. Has multiple bruises on her knees
d. Poor personal hygiene
Answer- d. Poor personal hygiene. Poor personal hygiene in a toddler is a potential indication of physical neglect. Because toddlers are still dependent on their parents for help with hygiene needs, poor personal hygiene indicates a lack of supervision.
A- The toddler has begun to develop a sense of body image and boundaries and can be resistant to intrusive assessments such as assessing the mouth or ears, or taking an axillary temperature. Therefore, this finding is not an indication of physical neglect.
B- Separation anxiety is an expected finding for a toddler. The child of this age can become
fearful and exhibit regressive behaviors when left alone with strangers and separated from her parents; therefore, this finding is not an indication of physical neglect.
C- The 18-month-old toddler has accomplished the gross motor skills of standing and walking and has begun to try to run but falls easily and can have bruises on her knees. Therefore, this finding is not an indication of physical neglect.
A nurse is caring for a school-age child who is receiving chemotherapy and is severely immunocompromised. Which of the following actions should the nurse take?
a. Use surgical asepsis when providing routine care for the child.
b. Administer the measles, mumps, rubella (MMR) vaccine to the child.
c. Screen the child's visitors for indications of infection.
d. Infuse packed RBCs.
Answer- c. Screen the child's visitors for indications of infection. The child who is severely immunocompromised is unable to adequately respond to infectious organisms resulting in the potential for overwhelming infection; therefore, the nurse should screen the child's visitors for
indications of infection.
A- It is not necessary for the nurse to use surgical asepsis when providing direct care. Strict hand washing and medical asepsis are recommended to prevent the spread of infection.
B- It is contraindicated for a child who is severely immunocompromised to receive the MMR vaccine because it is a live virus vaccine and the child may not be able to build adequate antibodies to prevent infection with the organism.
D- A child who is immunocompromised as a result of chemotherapy will have a decreased neutrophil count. The nurse should plan to infuse packed RBCs to the child who is anemic. However, packed RBCs will not increase the child’s neutrophil count.
N212 PEDS ATI PRACTICE B QUIZ
A nurse is teaching a school-age child who has a severe to bee venom and his parent about epinephrine. Which of the following instructions should the nurse include in the teaching?
allergy
a. Use a second dose if the first dose of epinephrine does not completely reverse the symptoms.
b. Store unused epinephrine syringes in the refrigerator.
c. Shake the epinephrine syringe prior to use to dissolve the precipitate.
d. Administer the medication subcutaneously in the back of the arm.
Answer- a. Use a second dose if the first dose of epinephrine does not completely reverse the symptoms. A biphasic response, in which the child will appear to recover and then experience a recurrence of symptoms, is possible with some allergic reactions. The nurse should instruct the parent and child to use a second dose if the first dose does not resolve all the symptoms.
B- The nurse should instruct the parent and child to store epinephrine in a dark area at room temperature. Refrigeration of an epinephrine syringe can result in failure of the injection
mechanism to work.
C- The nurse should instruct the child and his parent that the formation of precipitate or a brown coloration to the solution is an indication that the medication should be replaced and not used.
D- The nurse should instruct the child and his parent to inject the medication intramuscularly into the anterolateral aspect of the middle thigh.
A nurse is assessing a school-age child who has appendicitis with possible perforation. The nurse should identify which of the following as a manifestation of peritonitis?
a. Hyperactive bowel sounds
b. Abdominal distention
c. Bradycardia d. Polyuria
Answer- b. Abdominal distention. The nurse should recognize that abdominal distention is a manifestation of peritonitis. Peritonitis is an inflammation of the lining of the abdominal wall. This inflammation in the abdomen, along with the ileus that develops, causes abdominal distention.
A- Hypoactive bowel sounds are a manifestation of peritonitis. The peritoneal inflammation caused by the feces and bacteria released from the perforated appendix results in the development of an ileus, and a decrease in bowel motility.
C- Tachycardia is a manifestation of peritonitis resulting from infection and fluid shifts within the abdomen, which causes hypovolemia.
D- Polyuria occurs with an elevated glucose level and is not a manifestation of peritonitis.
N212 PEDS ATI PRACTICE B QUIZ
A nurse is reviewing the laboratory report of a 6-year-old child who is receiving chemotherapy. Which of the following laboratory values should the nurse report to the provider?
a. Hgb 8.5 g/dL
b. WBC 9,500/mm3
c. Prealbumin18 mg/dL
d. Platelets 300,000/mm3
Answer- a. Hgb 8.5 g/dL. The child receiving chemotherapy is at risk for anemia due to the chemotherapy effects on the blood forming cells of the bone marrow. The development of anemia is diagnosed through laboratory testing of hemoglobin and hematocrit levels. The nurse should recognize that a hemoglobin level of 8.5 g/dL is below the expected reference range for a 6-year-old child and should be reported to the provider.
B- The child receiving chemotherapy is at risk for infection due to the myelosuppressing effects of the medication used to treat the cancer. The presence of infection can be evaluated through
body temperature, redness, edema, warmth, or drainage of wound or IV sites, as well as through measurements of WBC and absolute neutrophil counts. A WBC count of 9,500/mm3 is within the expected reference range for a 6-year-old child.
C- The child receiving chemotherapy is at risk for malnutrition as a result of nausea and vomiting, stomatitis, and pain. Nutritional status can be evaluated through prealbumin, albumin, and transferrin levels. A prealbumin level 0f 18 mg/dL is within the expected reference range for a 6-year-old child.
D- The child receiving chemotherapy is at risk for hemorrhage due to the thrombocytopenic effects of the medications used to treat cancer. The development of thrombocytopenia is diagnosed through laboratory testing of platelet levels. A platelet count of 300,000/mm3 is within the expected reference range for a 6-year-old child.
A nurse is caring for a school-age child who is receiving a cefazolin via intermittent IV bolus. The child suddenly develops diffuse flushing of the skin and angioedema. After discontinuing the medication infusion, which of the following medications should the nurse administer first?
a. Prednisone
b. Epinephrine
c. Diphenhydramine d. Albuterol
Answer- b. Epinephrine. This child is most likely experiencing an anaphylactic reaction to the cefazolin. According to evidence-based practice the nurse should first administer epinephrine to treat the anaphylaxis. Epinephrine is a beta adrenergic agonist that stimulates the heart, causes vasoconstriction of blood vessels in the skin and mucous membranes, and triggers bronchodilation in the lungs.
N212 PEDS ATI PRACTICE B QUIZ
A- Prednisone is an anti-inflammatory agent that can treat severe inflammation Although it will benefit a child who is having an anaphylactic reaction, it is not the first medication the nurse should administer.
C- Even though histamines are not the major mediators of an anaphylactic reaction, administering an antihistamine such as diphenhydramine can help to decrease the allergic reaction. However, it is not the first medication the nurse should administer.
D- Albuterol is a beta adrenergic agonist that can treat acute bronchospasms. Although albuterol will improve the child's breathing, it is not the first medication the nurse should administer.
A nurse is caring for a school-age child who has diabetes mellitus and was admitted with a diagnosis of diabetic ketoacidosis. When performing the respiratory assessment, which of the following findings should the nurse expect?
a. Deep respirations of 32/min
b. Shallow respirations of 10/min
c. Paradoxic respirations of 26/min
d. Periods of apnea lasting for 20 seconds
Answer- a. Deep respirations of 32/min. The nurse should expect deep and rapid respirations in a child who has diabetic ketoacidosis. This respiratory rhythm is the body's attempt to blow off excess carbon dioxide and achieve a state of homeostasis.
B- The nurse should expect shallow respirations in a child who has respiratory depression related to opioid administration. However, shallow respirations are not an expected finding in a child who has ketoacidosis.
C- The nurse should expect paradoxic respirations in a child who has flail chest. However, paradoxic respirations are not an expected finding in a child who has ketoacidosis.
D- The nurse should expect periods of apnea in a child who has obstructive sleep apnea. However, periods of apnea are not an expected finding in a child who has ketoacidosis.
A nurse is caring for a newly-admitted school-age child who has hypopituitarism. Which of the following medications should the nurse expect the provider to recommend to the parents
for treating the child's condition?
a. Desmopressin
b. Luteinizing hormone-releasing hormone c. Recombinant growth hormone
d. Levothyroxine
Answer- c. Recombinant growth hormone. Recombinant growth hormone injections are used to treat hypopituitarism, which inhibits cell growth and results in growth failure. The nurse should expect the provider to recommend this treatment to the child's parents. The nurse's role is to provide emotional support for the parents as they make a decision about the treatment they
feel is best for their child.
A- Desmopressin is used to treat hyposecretion of antidiuretic hormones.
N212 PEDS ATI PRACTICE B QUIZ
B- Luteinizing hormone-releasing hormone is used in the treatment of precocious puberty to slow prepubertal growth in children and in the treatment of advanced prostate cancer in adult clients.
D- Levothyroxine is used to treat various hypothyroid conditions.
A nurse is preparing to administer a hepatitis B vaccine to a 1-month-old infant. The nurse should plan to inject the medication at which of the following locations?
Vastus lateralis
A is incorrect. The nurse should recognize that the deltoid muscle is used for intramuscular injections in infants age 18 months or older. The disadvantages associated with this site include the limited amount of medication that can be administered, as well as possible radial nerve damage.
B is incorrect. The nurse should realize that the abdomen is used for subcutaneous, rather than intramuscular, injections.
C is correct. The nurse should prepare to inject the vaccine into the vastus lateralis or anterolateral thigh muscle because this is a well-developed muscle in an infant and is linked with an improvement in immune response in comparison to other acceptable sites.
A nurse is caring for a toddler who is experiencing acute diarrhea and has moderate dehydration. Which of the following nutritional items should the nurse offer to the toddler? a. Apple juice
b. Peanut butter
c. Chicken broth
d. Oral rehydration solution
Answer- d. Oral rehydration solution. A toddler who has acute diarrhea should consume an oral rehydration solution to replace electrolytes and water and promote recovery from dehydration. A- A toddler who has acute diarrhea should not drink apple juice because it is high in carbohydrates and osmolarity and low in electrolytes.
B- A toddler who has acute diarrhea should not eat peanut butter because it is high in carbohydrates and fiber. The high sugar content can result in prolonging the diarrhea and
worsening of the dehydration, as water is pulled into the bowel lumen in response to the increased osmolality caused by the sugar. The fiber content further stimulates the bowel, worsening the diarrhea.
C- A toddler who has acute diarrhea should not consume chicken broth because it is high in sodium and is not nutrient-dense.
A nurse is teaching the parent of an infant who has a Pack harness to treat developmental dysplasia of the hip. The nurse should identify that which of the following statements by the parents indicates an understandings of the teaching?
a. "I should remove the harness at night to allow my infant to stretch her legs." b. "I will need to adjust the straps on the harness once each week."
N212 PEDS ATI PRACTICE B QUIZ
c. "I should apply baby powder to my infant's skin twice daily."
d. "I will place my infant's diapers under the harness straps."
Answer- d. "I will place my infant's diapers under the harness straps.". To prevent soiling of the harness the parent should apply the infant's diaper under the straps.
A- The harness is to be worn continuously until the hip is stable, which usually occurs within 6 to 12 weeks. Removing the harness frequently or for long periods of time will reduce the effectiveness of the treatment.
B- The Pavlik harness is designed to maintain the infant's hips in a position of flexion and abduction. The nurse should instruct the parents not to adjust the harness in any way to avoid complications.
C- The use of powders and lotions should be avoided during treatment with the Pavlik harness because these products in combination with the harness can cause skin irritation and breakdown.
A nurse is admitting a 4-month-old infant who has heart failure. Which of the following findings is the nurse's priority? (look at exhibit)
Vital Signs
Temperature 37.5° C (99.5°)
Heart rate 70/min
Respirations 30/min
Birth weight 3.2 kg (7 lb)
Current weight 5.9 (13 lb)
Flow Sheet
3 episodes of vomiting
6 wet diapers in 24 hr
Consumed 3 oz concentrated formula every 3 hr Medication Record
Digoxin 0.5 mcg PO Q12H
Furosemide 20 mg PO Q12H
a. Episodes of vomiting
b. Formula consumption
c. Weight
d. Temperature
Answer - a. Episodes of vomiting. When using the urgent vs. nonurgent approach to client care, the nurse determines that the priority finding is three episodes of vomiting. This can indicate digoxin toxicity, which requires immediate intervention; therefore, this is the priority finding.
B- A 4-month-old infant who has heart failure requires 3 to 4 oz of formula every 3 hr to adequately address caloric needs; therefore, there is another finding that is the nurse's priority. A feeding schedule of every 2 hr does not allow sufficient rest time between feedings, and a
feeding schedule of every 4 hr requires consumption of a higher volume, which is often not tolerated by the infant.
N212 PEDS ATI PRACTICE B QUIZ
C- A weight of 5.9 kg (13 lb) is an expected finding for a 4-month-old infant who weighed 3.2 kg (7 lb) at birth; therefore, there is another finding that is the nurse's priority. The infant should gain 680 g (1.5 lb) per month until the age of 5 months, and double his birth weight at the age
of 6 months.
D- A temperature of 37.5oC (99.5oC) is within the expected reference range for a 4 month-old infant; therefore, there is another finding that is the nurse's priority.
A nurse is providing discharge teaching to the parents of a 6-month-old infant who is postoperative following hypospadias repair with a stent placement. Which of the following instructions should the nurse include in the teaching?
a. "You may bathe your infant in an infant bathtub when you go home."
b. "Apply hydrocortisone cream to your infant's penis daily." c. "You should clamp your infant's stent twice daily."
d. "Allow the stent to drain directly into your infant's diaper."
Answer- d. "Allow the stent to drain directly into your infant's diaper." The nurse should instruct the parents to ensure that the stent drains directly into the infant's diaper to prevent kinking or twisting that can interfere with urine flow.
A- Submersing the stent in water can cause infection at the operative site. The parents should avoid placing the infant in an infant bathtub until after the provider removes the stent.
B- Following surgical repair of a hypospadias, the infant is at increased risk for infection at the operative site. The nurse should instruct the parents to apply an antibacterial ointment to the penis daily to help prevent infection.
C- The stent in place following hypospadias repair allows urine to drain from the body. The nurse should instruct the parents to avoid blocking the stent to prevent urinary stasis and potential injury to the infant.
A nurse is admitting an infant who has intussusception. Which of the following findings should the nurse expect?
a. Steatorrhea
b. Vomiting
c. Lethargy
d. Constipation
e. Weight gain
Answer - b. Vomiting, c. Lethargy.
Steatorrhea is incorrect. The nurse should expect the infant with intussusception to have bloody stools that are currant jelly-like in appearance. Steatorrhea is bulky, fatty stools, and is a manifestation of cystic fibrosis.
Vomiting is correct. The nurse should expect the infant with intussusception to exhibit vomiting
due to the obstruction that occurs when a segment of the bowel telescopes within another segment of the bowel.
N212 PEDS ATI PRACTICE B QUIZ
Lethargy is correct. The nurse should expect the infant with intussusception to exhibit lethargy due to episodes of severe pain during which the infant cries inconsolably leading to exhaustion and decreased nutritional intake.
Constipation is incorrect. The nurse should expect the infant with intussusception to have mucus-filled and currant jelly-like diarrhea due to the leaking of blood and mucus into the intestinal lumen.
Weight gain is incorrect. The nurse should expect the infant with intussusception to have weight loss due to anorexia and episodes of vomiting and diarrhea.
A nurse is providing teaching to the parent of a preschooler about ways to prevent acute asthma attacks. Which fo the following statements by the parent should the nurse identify as understanding the teaching?
a. "I will use a humidifier in my child's room at night."
b. "I will give my child a cough suppressant every six hours if he has a cough."
c. "I should avoid using a wet mop on my floors when I am cleaning."
d. "I should keep my child indoors when I mow the yard."
Answer- d. "I should keep my child indoors when I mow the yard." The nurse should instruct the parent to keep the preschooler indoors during lawn maintenance or when the pollen count is increased. Guarding against exposure to known allergens found outdoors, such as grass, tree, and weed pollen, will decrease the frequency of the preschooler's asthma attacks.
A- Dehumidifiers or air conditioners are recommended to control the room temperature because heat and humidification can cause an asthma exacerbation.
B- Cough suppressants are contraindicated for children who have asthma because they need to be able to cough up mucus to keep their airway open.
C- The parent should wet mop bare floors weekly because sweeping floors can trigger an asthma attack due to the inhalation of the dust that becomes airborne during sweeping.
A nurse is providing discharge teaching to the parents of a Caucasian toddler who had a lower leg cast applied 24 hr ago. The nurse should instruct the parents to report which of the following findings to the provider?
a. Capillary refill time less than 2 seconds
b. Restricted ability to move the toes
c. Swelling of the casted foot when the leg is dependent d. Toes that are deep pink in color
Answer- b. Restricted ability to move the toes. The nurse should inform the parents that a restricted ability of the toddler to move his toes is a sign of neurovascular compromise and requires immediate notification of the provider. Permanent muscle and tissue damage may occur in just a few hours.
A- Capillary refill time is assessed to determine circulatory status by pressing lightly on the tips
of the toes until the skin has blanched. A capillary refill time that is greater than 2 seconds indicates circulatory compromise and should be reported to the provider immediately.
N212 PEDS ATI PRACTICE B QUIZ
C- Swelling of the casted foot when the leg is dependent is an expected finding. The nurse should instruct the parents that frequent rest is needed for the next several days, and that the casted foot should not be in a dependent position for more than 30 min. When the toddler is
resting, the casted extremity should be elevated on a pillow at chest level to minimize swelling. D- Toes that are deep pink in color is an expected finding for a Caucasian toddler and does not warrant provider notification.
A nurse is planning care for a school-age-child who is in the oliguric phase of acute kidney injury (AKI) and has a sodium level of 129 mEq/L. Which of the following interventions should the nurse include in the plan?
a. Administer ibuprofen to the child for a temperature greater than 38o C (101o F).
b. Assess the child's blood pressure every 8 hr.
c. Weigh the child weekly at various times of the day.
d. Initiate seizure precautions for the child.
Answer- d. Initiate seizure precautions for the child. A sodium level of 129 mEq/L indicates hyponatremia and places the child at increased risk for neurological deficits and seizure activity. The nurse should complete a neurologic assessment and implement seizure precautions in order to maintain the child's safety.
A- A child who has AKI can develop a fever due to an infection. Because AKI is a contraindication to receiving medications that are nephrotoxic, such as NSAIDs, the nurse should use compensatory measures, such as turning on a fan in the room.
B- A child who has AKI often is hypertensive due to fluid volume excess and the activation of the renin-angiotensin system. To prevent complications, such as hypertensive encephalopathy, the nurse should assess the child's blood pressure every 4 to 6 hr.
C- In the oliguric phase of AKI, the child will have decreased urine output and fluid retention. This can result in water intoxication, which predisposes the child to neurologic alterations, such as seizures. To ensure accurate evaluation of fluid balance, the nurse should plan to weigh the child daily, at the same time, in the same clothing and using the same scale.
A nurse is assessing a 6-month-old infant as a visit. Which of the following should the nurse report to the provider?
a. Presence of strabismus
b. Presence of corneal light reflex
c. Presence of open anterior fontanel d. Presence of cerumen
Answer- a. Presence of strabismus. Strabismus, or crossing of the eyes, disappears at 3 - 4 months of age. Therefore, the nurse should report this finding to the provider.
B- The nurse should recognize that the presence of a corneal light reflex is an expected finding
well-infant
and is not necessary to report to the provider.
N212 PEDS ATI PRACTICE B QUIZ
C- The nurse should recognize that the presence of an open anterior fontanel is an expected finding and is not necessary to report to the provider.
D- The nurse should recognize that the presence of cerumen is an expected finding and is not
necessary to report to the provider.
A nurse is planning care for a school-age child who has a tunneled central venous access device. Which of the following interventions should the nurse include in the plan?
a. Use sterile scissors to remove the dressing from the site.
b. Irrigate each lumen weekly with 10 mL of 0.9% sodium chloride solution when not in use. c. Access the site using a noncoring angled needle.
d. Use a semipermeable transparent dressing to cover the site.
Answer- d. Use a semipermeable transparent dressing to cover the site. The nurse should cover the site with a semipermeable transparent dressing to reduce the risk of infection.
A- The nurse should avoid the use of scissors when performing dressing changes because this
can result in accidental cutting of the catheter.
B- The nurse should flush each lumen of the catheter with a heparin solution daily when not in use.
C- The nurse should use a noncoring angled or straight needle when accessing an implanted port.
A nurse is creating a plan of care for a school-age child who has heart disease and has developed heart failure. Which of the following interventions should the nurse include in the plan?
a. Provide small, frequent meals to the child.
b. Schedule time in the play room for the child.
c. Weigh the child weekly.
d. Maintain the child in a supine position.
Answer- a. Provide small, frequent meals to the child. The metabolic rate for a child who has
heart failure is high because of poor cardiac function. Therefore, the nurse should provide small, frequent meals to the child because it helps to conserve energy.
B- The nurse should restrict play activities to the child's bed to minimize energy expenditure. C- The nurse should weigh the child daily.
D- To provide for maximum chest expansion, the nurse should maintain the bed in a semi- Fowler's position while the child is in bed.
A nurse in an emergency department is caring for a school-age child who has sustained a superficial minor burn from fireworks on his forearm. Which or the following actions should
the nurse take?
a. Administer a tetanus toxoid if more than 1 year since prior dose.
N212 PEDS ATI PRACTICE B QUIZ
b. Use an antimicrobial ointment on the affected area.
c. Leave the burn area open to air.
d. Place an ice pack on the affected area.
Answer- b. Use an antimicrobial ointment on the affected area. The nurse should apply an antimicrobial ointment to the burned area to prevent infection.
A- The nurse should administer a tetanus toxoid if it has been more than 5 years since the prior dose.
C- The nurse should apply a clean-dry dressing of fine mesh gauze and a light gauze dressing that restricts movement to prevent injury to the wound.
D- Applying ice to the affected area may impair circulation to the area and increase tissue damage.
A nurse is caring for a school-age who has acute rheumatic fever. Which of the following actions should the nurse take?
a. Limit the child's sodium intake.
b. Place a "no visitors" sign on the child's door. c. Maintain the child on bed rest.
d. Avoid administering salicylates to the child.
Answer- c. Maintain the child on bed rest. The nurse should maintain the child on bed rest as well as limit the child's activity during the acute phase of rheumatic fever to assist with the prevention of cardiac damage.
A- Rheumatic fever is an inflammatory disease resulting from an immune response that involves the heart, joints, skin, and central nervous system. Therefore, there is no indication or benefit to limiting the child's sodium intake.
B- Rheumatic fever is not contagious to others. Therefore, unless it is requested by the parents or child, it is not necessary to restrict visitors.
D- The nurse should administer salicylates to the child who has acute rheumatic fever to decrease fever and discomfort and help to control the inflammatory process.
A nurse in an emergency department is auscultating the lungs of an adolescent who is experiencing dyspnea. The nurse should identify the sound as which of the following (audio clip)?
a. Wheezes
b. Crackles
c. Pleural friction rub d. Rhonchi
Answer- a. Wheezes. The nurse should identify the sound during auscultation as wheezes, which are high-pitched, musical or whistling-like sounds heard primarily on expiration as air
passes through and vibrates narrowed airways.
N212 PEDS ATI PRACTICE B QUIZ
B- Crackles are high-pitched, short, and noncontinuous sounds heard usually at the end of inspiration. Crackles occur when air expands deflated alveoli or when the passage of air through small airways is disrupted.
C- A pleural friction rub is a loud, rough, grating sound and can be heard during inspiration or expiration. A pleural friction rub occurs when the pleurae are inflamed and the surfaces rub together.
D- Rhonchi are low-pitched, continuous sounds that have a snore-like quality and are usually louder during expiration. Rhonchi occur when the larger airways are obstructed.
Read More