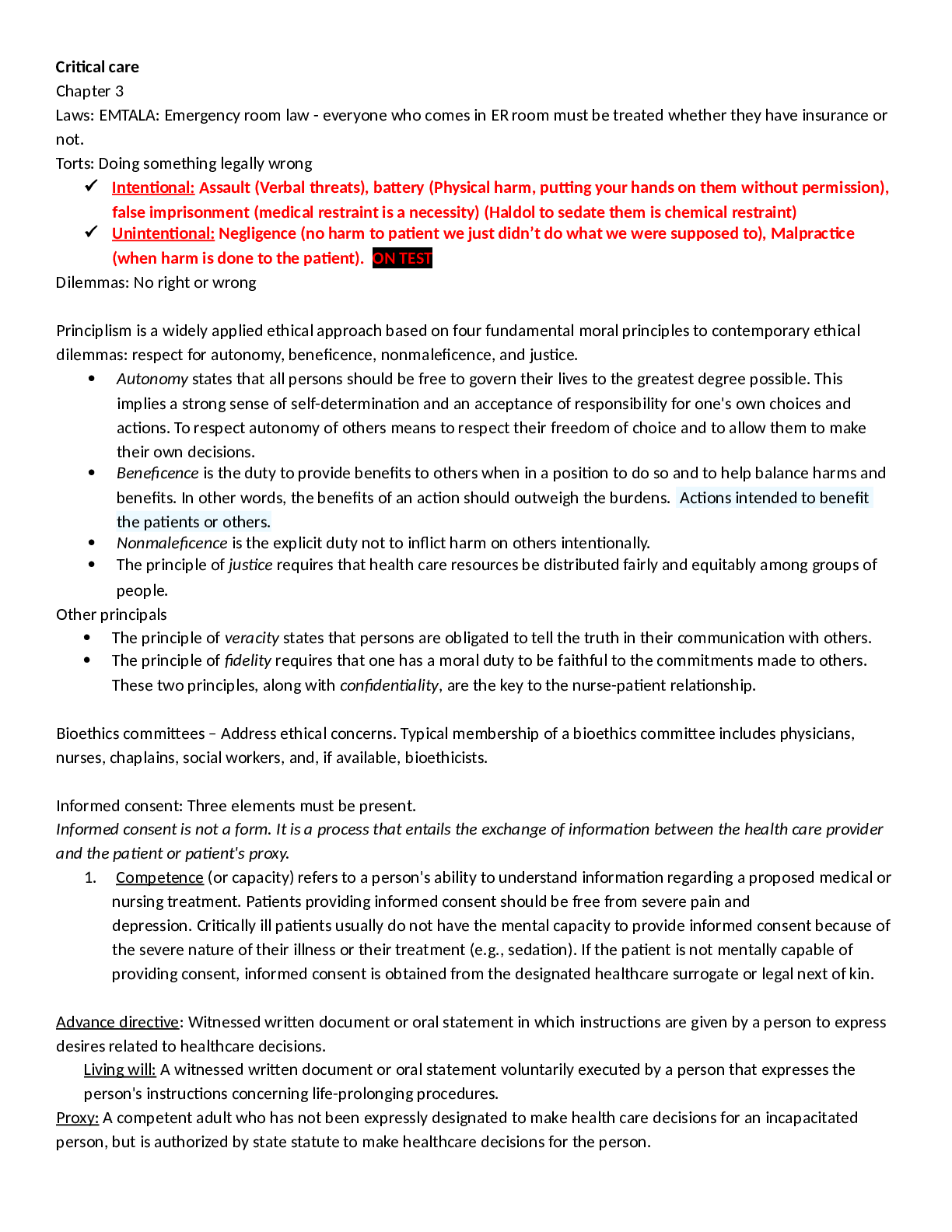
Critical care Chapter 3 Laws EMTALA: Emergency room law - everyone who comes in ER room must be treated whether they have insurance or not.
Course
Philosophy
Subject
Chemistry
Category
Study Guide
Pages
47
Uploaded By
ATIPROS
Preview 5 out of 47 Pages
.png)
Download all 47 pages for $ 14.00
Reviews (0)
$14.00
