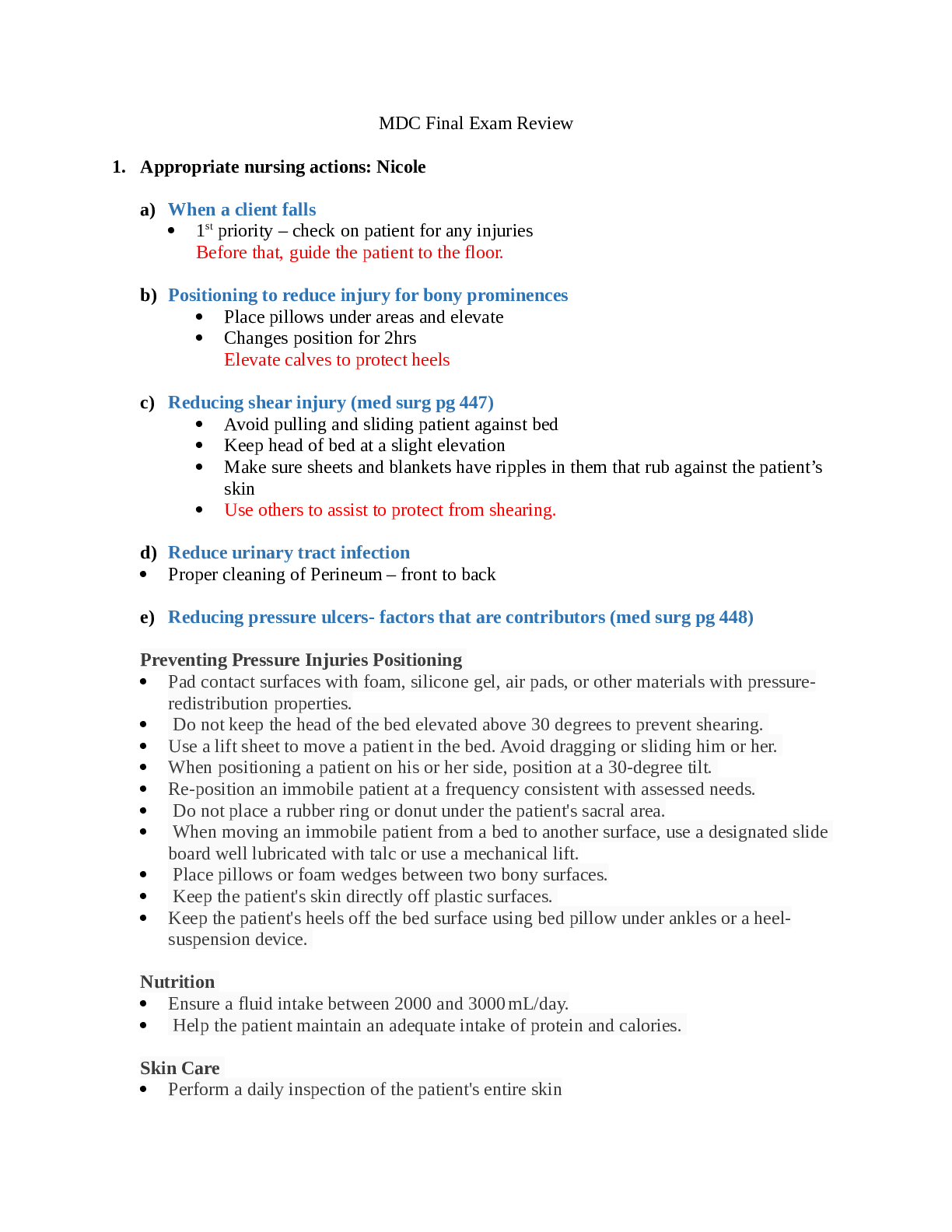
MDC Final Exam Review
1. Appropriate nursing actions: Nicole
a) When a client falls
1
st priority – check on patient for any injuries
Before that, guide the patient to the floor.
b) Positioning to reduce injury for bony prominences
Place pillows under areas and elevate
Changes position for 2hrs
Elevate calves to protect heels
c) Reducing shear injury (med surg pg 447)
Avoid pulling and sliding patient against bed
Keep head of bed at a slight elevation
Make sure sheets and blankets have ripples in them that rub against the patient’s
skin
Use others to assist to protect from shearing.
d) Reduce urinary tract infection
Proper cleaning of Perineum – front to back
e) Reducing pressure ulcers- factors that are contributors (med surg pg 448)
Preventing Pressure Injuries Positioning
Pad contact surfaces with foam, silicone gel, air pads, or other materials with pressureredistribution properties.
Do not keep the head of the bed elevated above 30 degrees to prevent shearing.
Use a lift sheet to move a patient in the bed. Avoid dragging or sliding him or her.
When positioning a patient on his or her side, position at a 30-degree tilt.
Re-position an immobile patient at a frequency consistent with assessed needs.
Do not place a rubber ring or donut under the patient's sacral area.
When moving an immobile patient from a bed to another surface, use a designated slide
board well lubricated with talc or use a mechanical lift.
Place pillows or foam wedges between two bony surfaces.
Keep the patient's skin directly off plastic surfaces.
Keep the patient's heels off the bed surface using bed pillow under ankles or a heelsuspension device.
Nutrition
Ensure a fluid intake between 2000 and 3000 mL/day.
Help the patient maintain an adequate intake of protein and calories.
Skin Care
Perform a daily inspection of the patient's entire skin
Document and report any manifestations of skin infection.
Use moisturizers daily on dry skin and apply when skin is damp
Keep moisture from prolonged contact with skin:
Dry areas where two skin surfaces touch, such as the axillae and under the breasts.
Place absorbent pads under areas where perspiration collects.
Use moisture barriers on skin areas where wound drainage or incontinence occurs.
Do not massage bony prominences.
Humidify the room.
Skin Cleaning
Clean the skin as soon as possible after soiling occurs and at routine intervals.
Use a mild, heavily fatted soap or gentle commercial cleanser for incontinence.
Use tepid rather than hot water.
In the perineal area, use a disposable cleaning cloth that contains a skin-barrier agent.
While cleaning, use the minimum scrubbing force necessary to remove soil.
Gently pat rather than rub the skin dry.
Do not use powders or talc directly on the perineum.
After cleaning, apply a commercial skin barrier to areas in frequent contact with urine or
feces.
f) For vital signs out of range (i.e low oxygen saturation) (module 1 slide 56-59)
Normal body temperature 96.4 to 99.5 (depending on the site)
Respiration Rate – 12 to20 breaths per minute
BP – 120/80 and below; anything higher is abnormal
Pulse-Oximetry (saturation) – 94 to 100%
Pulse – 60 to 100 BPM
g) Appropriate measures in taking an oral temperature (module 1 slides55)
h) Vital signs that can indicate post-surgical pain?
Elevated Heart Rate
Breathing rate can be elevated
Elevated BP
2. Describe the following: Nicole
a) Complications of amputations and type of pain (module 1 slide 10)
Possibility of phantom pain
b) Autonomy for a client requiring oral care (funds book pg 594-595)
Brush the teeth twice a day.
Use a soft toothbrush.
Moisturize oral mucosa and lips every 2 to 4 hours.
Use a chlorhexidine gluconate (0.12%) rinse twice a day during the perioperative period
for patients who undergo cardiac surgery (adult patients).
Use mouthwash inside the mouth twice a day for adult patients who are on a ventilator.
Give the patients the oral supplies
c) Fire safety measures and priorities (module 3 slides 12 &22)
o Fires
Home fires are the major cause of death and injuries
Older adults & children < 5y/o have the highest risk.
Most common causes of fires:
Cooking fires
Smoking
Heating Equipment
Home oxygen administration equipment: 75% of home fires involves
oxygen, smoking materials are the ignition source
Remove the client from the area
o RACE
Rescue – remove patient from danger
Alarm – pull the alarm
Contain - close doors
Extinguish fire (if possible)
o PASS
Pull the pin
Aim at the base of the fire
Squeeze the handles
Sweep back and forth
d) Infant safety- education for new moms in keeping babies safe.
Don’t Sleep with baby
Car seat faces backwards for 2 years
Baby should sleep in their back
Do not use microwave to heat formula
Do not sleep with mom and dad
e) Client orientation to a new room may include what specifics
Ensure they can use call light before you leave
Show them where their personal items are and place them near to them
Show them where all the furniture is at and walk them around it.
Also show them where the bathroom is and how to get to it
f) Delegation to an unlicensed assistive personnel (UAP)
o Anytime there is concern over a finding from an unlicensed person – assess the
patient yourself to confirm the concern
o Things that can be delegated to unlicensed personnel
Vital signs on a non-critical patient
Moving/ambulating a patient
Bedside glucose monitoring
Bathing and documenting tasks
3. Describe the following: Casey
a) Benefits of bathing for a client
Cleans the body, stimulates circulation, provides relaxation, and enhance healing.
b) Caring for a patient with dementia, specific nursing interventions
promote patient orientation, use simple communication, decrease anxiety, keep the
patient safe, and pro- vide continuity of care. (fund book, p. 787). As for assistance with
procedures such as indwelling catheters or IV insertions.
c) Normal temperatures of clients of all ages (infants, adults, elderly)
Infant 97.7- 99.5, Adults 96.4 to 99.5, Elderly 96.8 average (due to loss of subcutaneous
fat)
d) Main causes of accidental poisoning
Young Children exposure is mainly due to improper storage of household
chemicals, medicines, vitamins & cosmetics
Older children and adolescents cause is due to suicide attempt, accidental
experiment with recreational or prescription drugs.
Adults poisoning occurs by misuse or abuse or prescription drugs, especially
narcotics, tranquilizers and antidepressants ( module 3 , slide 8)
e) Main purpose of incident report
To give the health care facility and the healthcare professionals the opportunity to address
the issue and prevent the occurrence of future incidents.
f) Interventions for a patient with a DVT
Patient education
Leg exercises
Early ambulation
Adequate hydration
Graduated compression stockings
Intermittent pneumatic compression, such as sequential compression devices (SCDs)
Venous plexus foot pump
Anticoagulant therapy ( med surg p. 744)
g) Different types of nurse/client relationships
Pre-interaction: The student nurse gathers information about the client before having a
personal interaction, looking at the client’s medical record to begin data collection.
Orientation: The student nurse introduces themselves, explains their role in the
relationship, determines the name the client wishes to be addressed by, and establishes
trust and rapport.
Working: Active part of the relationship. The student nurse communicates caring and
compassion to the client, encourages the client to express concerns and feelings openly
and honestly in an environment, and shows mutual respect and understanding. The
professional relationship is competent, courteous, and confidential.
Termination: This marks the end of the relationship, whether at the end of the shift or at
discharge. The student nurse summarizes all of the work done during the relationship.
This is a good way to end the shift.
4. Communication: Casey
what are important aspects in communication?
a) Christian Scientist beliefs in the ED
Will most likely only encounter these patients following an accident because they do
follow Western Medicine as first choice to promote health. Most adults are not likely to
accept a blood transfusion. ( funds p. 332)
b) Asian cultures and space
People stand farther apart and touch less
c) Jehovah’s Witness and blood transfusions
View accepting blood transfusions or blood products as morally wrong. ( funds p. 332).
However, it is vital for the nurse to educate o the client on the reasons why the blood
transfusion is needed.
d) Hindu clients and bathing
Hindus prefer to wash in free-flowing water (e.g., a shower instead of a tub bath). If a
shower is not avail- able, provide a jug of water for the person to use in the bath. Women
are modest and usually prefer to be treated by female medical staff (funds p. 333)
e) Catholics and last rights- who does the nurse communicate to?
A Roman Catholic who is seriously ill might wish to receive the sacrament of anointing
the sick. This sacrament, once known as the last rites, can be repeated if the person
recovers and then be- comes ill at a later time. Only a priest can hear the sacrament of
reconciliation (confession), during which God, through the agency of the priest, grants
forgiveness for past sins. (funds p. 332)
f) Describe empathetic statements
Desire to understand and be sensitive to feelings, beliefs and situation.
o As the nurse, adaptation to different style, tone, vocabulary and behavior is
important to create the best approach for each patients’ situation.
Place your-self in the patient situation. Think about “how would I want to be treated if it
was me? This will help you:
o Appreciate everyone uniqueness
o Understand the needs (module 2, slide 13)
g) Describe therapeutic communication
Client-centered communication directed to achieve the patients’ goal.
Has 5 key characteristics
Key skills to establish a therapeutic relationship, express interest, concern, caring
perception, provide and obtain healthcare information (module 2, slide 12)
h) How can communication be improved with a client wearing hearing aids?
Position yourself directly in front of the patient.
Ensure that you are not sitting or standing in front of a bright light or window, which can
interfere with the patient's ability to see your lips move.
Make sure that the room is well lighted.
Get the patient's attention before you begin to speak.
Move closer to the better-hearing ear.
Speak clearly and slowly.
Do not shout (shouting often makes understanding more difficult).
Keep hands and other objects away from your mouth when talking to the patient.
Have conversations in a quiet room with minimal distractions.
Have the patient repeat your statements, not just indicate assent.
Rephrase sentences and repeat information to aid understanding.
Use appropriate hand motions.
Write messages on paper if the patient is able to read. (med surg p.999)
Remove distractions like turning off the television.
i) Non-compliant clients- what are best responses by the nurse?
Find out the reason why. Provide education. Document.
j) How can a nurse best meet psychosocial needs for a client?
involve clients in daily care
Provide stimuli such as newspapers, TV, magazines
Assist with grooming and hygiene such as shaving and makeup
Involve the client in planning of daily routine
Maintain orientation to time such as a clock, and calendar
5. Immobility/mobility: Janett
What exercises can improve mobility?
Range of motion (Passive & Active) Weight baring exercise (page 208)
Describe different types of passive range of motion exercises.
(flexion, extension, abduction, adduction, circumduction, internal/external rotation, opposition)
(page 506)
Explain why certain medications place clients at risk for pressure ulcers.
Some medications alter the blood flow. This causes less blood to go to pressure areas. May lead
to necrosis. (page 81)
What are the benefits of exercise?
Bone reformation and growth, Cardiovascular health promotion, Promotes balance and stability,
Reduce stress and increase energy levels, Improves pulmonary circulation, skeletal development,
skin tone, Reduces systemic inflammation (page 187)
What are the negative effects of immobility?
Osteoarthritis, Rheumatoid Arthritis, Loss of muscle strength, Impaired balance, Altered join
mobility, Decreased stability, Osteoporosis, Depression, isolation, anxiety, and mood change,
Can cause decreased peristalsis, DVT(page 830)
Interventions to reduce the risk of contractures
Gently straighten out contracted extremity, fingers, Mobility-encouraging interventions such as
passive ROM, and rotation. Flexion and extension exercises, These interventions should be
performed about every 2hrs and as needed if the contractures are present (page 843)
What are the effects of immobility on the respiratory system?
Pulmonary embolisms, pneumonia. Decreased depth of respirations, decreased ability to cough,
atelectasis (page 831)
6. Diseases that contribute to immobility: Janett
Assessment of osteoarthritis.
progressive deterioration & loss of cartilage & bone in one or more joints (crepitus), history
(of join pain, pain management, history of joint injury, weight history, family history,
affecting of the ADL’s), atrophy of skeletal muscle from disuse, limp, lab assessment
(erythrocyte sedimentation rate, c-reactive protein) (page 306)
Non-pharmacological interventions for rheumatoid arthritis.
Adequate rest, proper positioning, heat/cold therapy, hypnosis, imagery, music therapy,
adequate nutrition, gradual weight loss (page 323)
Education of a client using a walker from a lying/sitting position.
Feet firmly on the floor, one hand on the chair the other on the walker. Stand up slowly. (page
845)
Education on reducing risk of osteoporosis.
Prevent obesity, proper nutrition, avoid injuries, weight baring exercises, active live style,
avoid staying (siting or laying) in one stop for too long, participate in ADLs (page 212).
Know why these interventions are important.
7. Osteomyelitis (infection of the bone. Can be acute or chronic): Angela
interventions in reducing infection:
a) Proper dental care
b) Maintaining clean & intact skin
c) Proper hand hygiene
d) Not leaving catheters in long tern
e) Understanding who is at risk
f) Using proper standard and contact precautions
g) Reduce caffeine and stop smoking (Module 5 PPT; slide 49)
Open fractures- interventions in reducing infection
Hand washing or strict infection control
Dressing changes with aseptic technique
Monitor vital signs especially temperature & HR
Administer broad spectrum antibiotics if ordered (Clindamycin & Gentamycin)
If irrigating open wound may be used using an antibiotic solution (Module 6 PPT;
slide 23)
For chronic infections – adherence to antibiotic regimen
Priorities in discharge instructions for osteomyelitis
4-6 weeks of antibiotic therapy for acute osteomyelitis
May require wound irrigation & medicated beads that are directly in contact with the
wound
May be in contact isolation precautions if area is draining copious amounts of
drainage
Hyperbaric oxygen therapy (Module 5 PPT; slide 50)
8. Describe the following: Angela
How does a nurse perform a neurovascular assessment? If negative findings occur, what
should the nurse do next?
Assessment of the extremities to evaluate sensory & motor function (neuro) & peripheral
circulation (vascular). Components: (bilateral comparison) pulses, capillary refill, skin color,
temperature, sensation, & motor function (movement). Pain & edema are also assessed. (5
P’s: Pain, Pulse, Pallor, Paresthesia, & Paralysis) A doppler is used to determine blood flow.
(Module 5 PPT; slide 15)
Negative findings:
a. Assess BAC & provide as needed
b. Expose the area of injury to assure accurate assessment
c. Control any bleeding. Apply direct pressure to bleeding site or pressure artery above
the fracture
d. To prevent shock, position patient in a supine
e. Splint the injury
Read More