Advanced Physical Assessment & Diagnostic Reasoning - August '18, NURS 607
Return to Assignment
Self-Reflection
Activity Description: These prompts help you think more deeply about your performance in the assignment. Reflective writing develops your
clinical reasoning skills as you grow and improve as a clinician, and gives your instructor insight into your learning process. The more detail and
depth you provide in your responses, the more you will benefit from this activity.
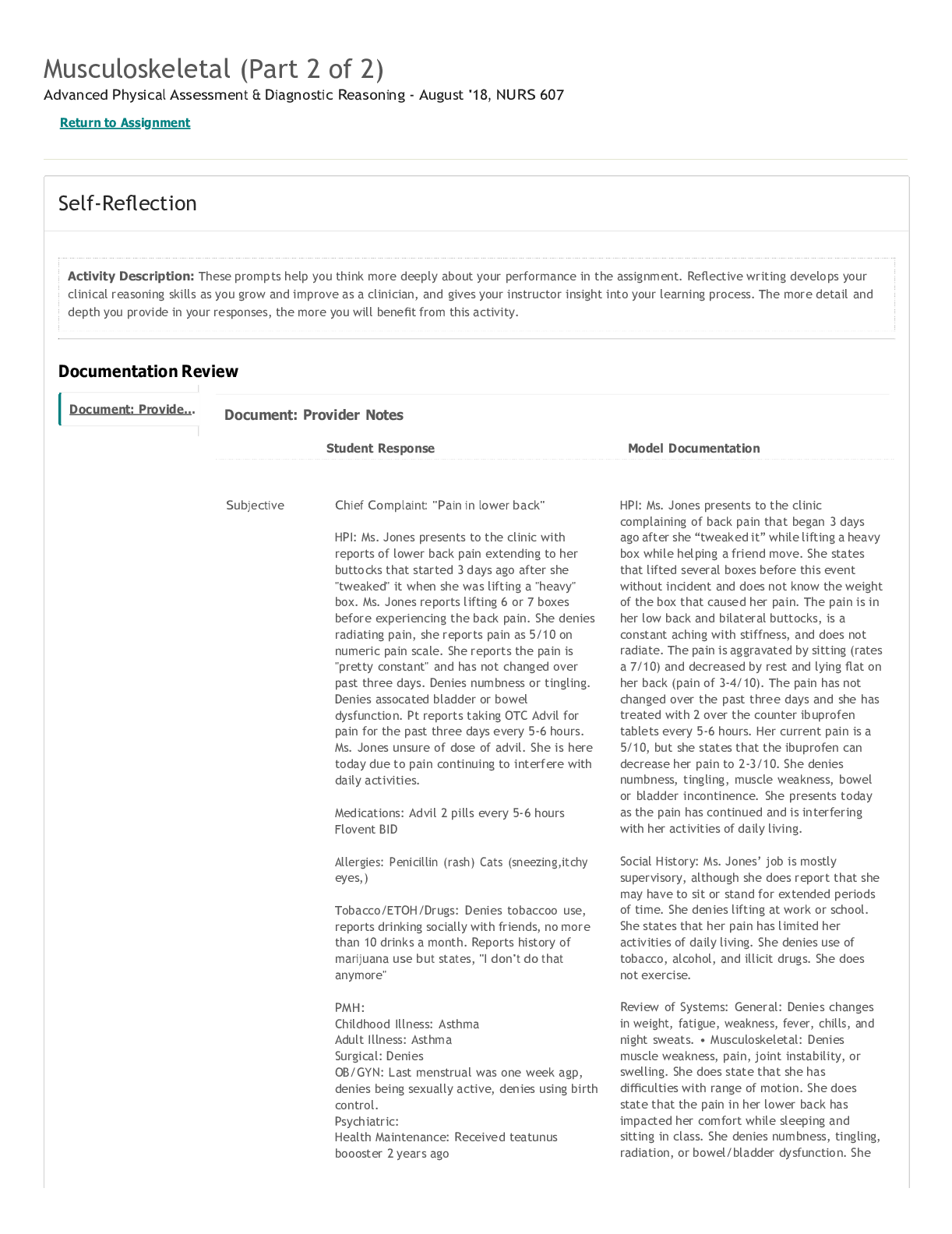
Documentation Review
Document: Provider Notes
Student Response Model Documentation
Subjective Chief Complaint: "Pain in lower back"
HPI: Ms. Jones presents to the clinic with
reports of lower back pain extending to her
buttocks that started 3 days ago after she
"tweaked" it when she was lifting a "heavy"
box. Ms. Jones reports lifting 6 or 7 boxes
before experiencing the back pain. She denies
radiating pain, she reports pain as 5/10 on
numeric pain scale. She reports the pain is
"pretty constant" and has not changed over
past three days. Denies numbness or tingling.
Denies assocated bladder or bowel
dysfunction. Pt reports taking OTC Advil for
pain for the past three days every 5-6 hours.
Ms. Jones unsure of dose of advil. She is here
today due to pain continuing to interfere with
daily activities.
Medications: Advil 2 pills every 5-6 hours
Flovent BID
Allergies: Penicillin (rash) Cats (sneezing,itchy
eyes,)
Tobacco/ETOH/Drugs: Denies tobaccoo use,
reports drinking socially with friends, no more
than 10 drinks a month. Reports history of
marijuana use but states, "I don't do that
anymore"
PMH:
Childhood Illness: Asthma
Adult Illness: Asthma
Surgical: Denies
OB/GYN: Last menstrual was one week agp,
denies being sexually active, denies using birth
control.
Psychiatric:
Health Maintenance: Received teatunus
boooster 2 years ago
HPI: Ms. Jones presents to the clinic
complaining of back pain that began 3 days
ago after she “tweaked it” while lifting a heavy
box while helping a friend move. She states
that lifted several boxes before this event
without incident and does not know the weight
of the box that caused her pain. The pain is in
her low back and bilateral buttocks, is a
constant aching with stiffness, and does not
radiate. The pain is aggravated by sitting (rates
a 7/10) and decreased by rest and lying flat on
her back (pain of 3-4/10). The pain has not
changed over the past three days and she has
treated with 2 over the counter ibuprofen
tablets every 5-6 hours. Her current pain is a
5/10, but she states that the ibuprofen can
decrease her pain to 2-3/10. She denies
numbness, tingling, muscle weakness, bowel
or bladder incontinence. She presents today
as the pain has continued and is interfering
with her activities of daily living.
Social History: Ms. Jones’ job is mostly
supervisory, although she does report that she
may have to sit or stand for extended periods
of time. She denies lifting at work or school.
She states that her pain has limited her
activities of daily living. She denies use of
tobacco, alcohol, and illicit drugs. She does
not exercise.
Review of Systems: General: Denies changes
in weight, fatigue, weakness, fever, chills, and
night sweats. • Musculoskeletal: Denies
muscle weakness, pain, joint instability, or
swelling. She does state that she has
difficulties with range of motion. She does
state that the pain in her lower back has
impacted her comfort while sleeping and
sitting in class. She denies numbness, tingling,
radiation, or bowel/bladder dysfunction. She
Document: Provide...
9/7/2018 Musculoskeletal | In Progress Attempt | Shadow Health
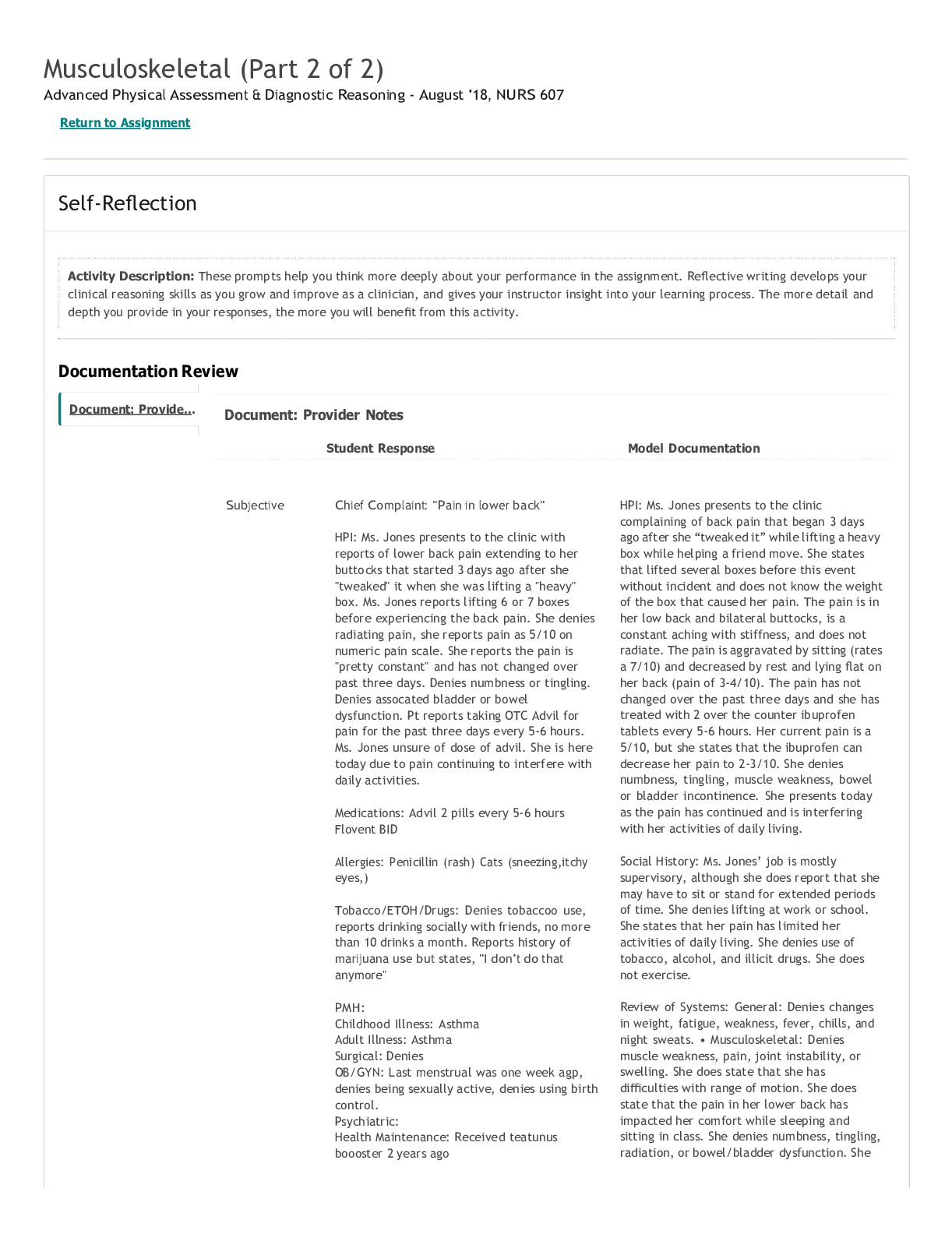
Student Response Model Documentation
muscle disorders, Father died in car accident,
mother living, medical history includes high
cholesterol and hypertension, sister living,
medical history of asthma, brother living, pt
reports, "He's a little big"
Personal/Social Hx: Currently enrolled in
bachelor's degree program, works as a
supervisor at Mid-American Copy and Ship,
enjoys dacing and watching TV in spare time.
Lives at home with mother and sister.
ROS:
General: Denies changes in weight, fatigue and
recent fever
Skin: Pt reports skin around neck getting
darker and recent skin breakout
Head: Denies headache, recent head injury,
dizziness
Eyes: Denies wearing glasses/contacts, reports
last eye exam was as a child, reports blurry
vision with reading
Ears: Denies hearing difficulties
Nose: Denies issues with nose
Throat: Denies issues with
chewing/swallowing, last dental exam a few
years ago
Neck: Denies swollen glands/neck stiffiness
CV: Denies chest pain, reports chest tightness
with asthma
GI: Reports last bowel movement last night,
denies changes in appetite
Urinary: Denies difficulty urinating
MSK: Denies joint pain, swelling or stiffiness.
Reports low back pain that does not radiate,
reports low back pain is making activities of
daily living harder, reports " I can't really sit or
move alot"
Psychiatric: Denies thoughts or feeling
down/depressed/hopeless
Neurologic: Denies numbness tingling, denies
changes in memory, denies fainting and
seizure activity
Endocrine: Denies heat/cold intolerance,
denies family history of thyroid disorders.
Read More