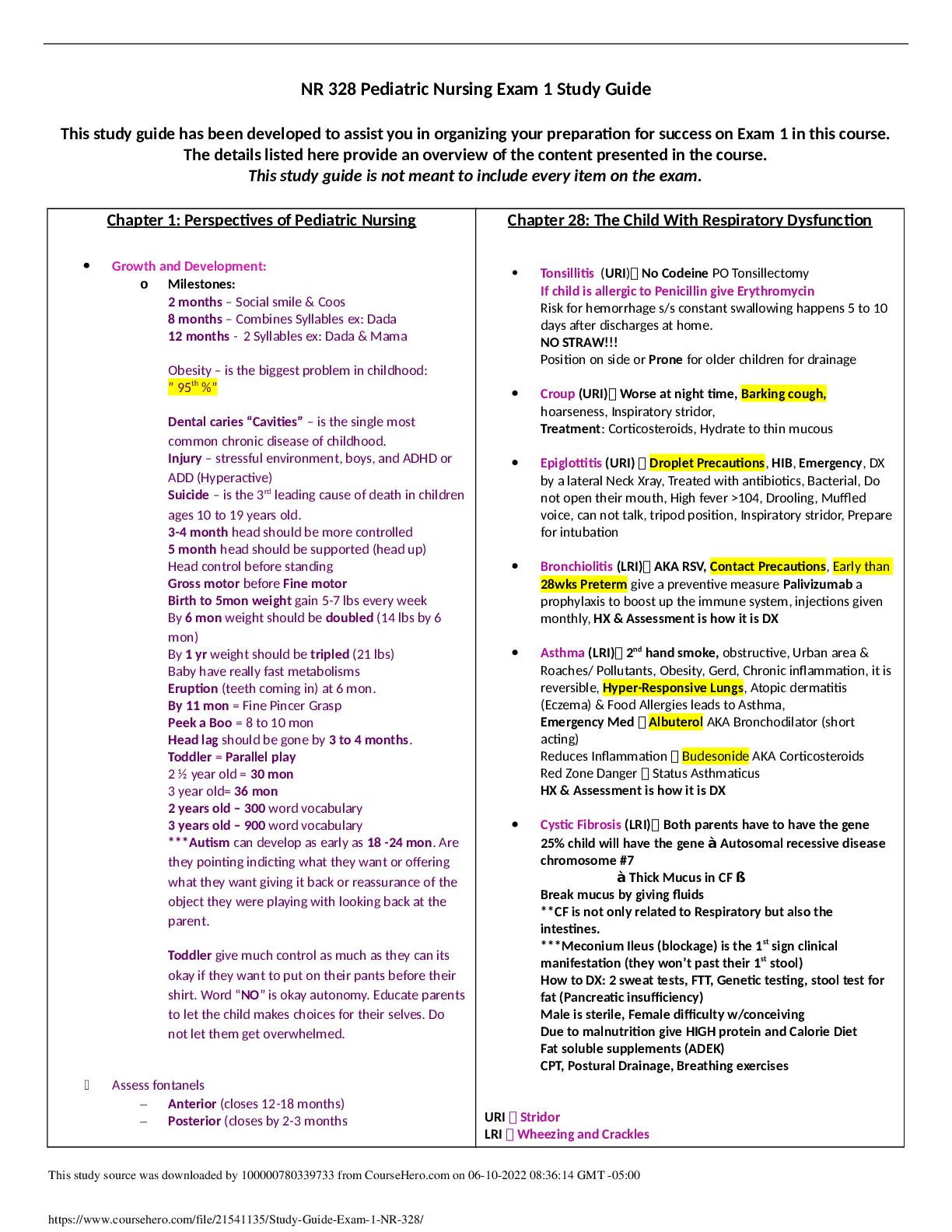
This study guide has been developed to assist you in organizing your preparation for success on Exam 1 in this course.
The details listed here provide an overview of the content presented in the course.
This study guide is not meant to include every item on the exam.
Chapter 1: Perspectives of Pediatric Nursing
Chapter 28: The Child With Respiratory Dysfunction
Growth and Development:
o Milestones:
2 months – Social smile & Coos
8 months – Combines Syllables ex: Dada
12 months - 2 Syllables ex: Dada & Mama
Obesity – is the biggest problem in childhood:
” 95th %”
Dental caries “Cavities” – is the single most
common chronic disease of childhood.
Injury – stressful environment, boys, and ADHD or
ADD (Hyperactive)
Suicide – is the 3rd leading cause of death in children
ages 10 to 19 years old.
3-4 month head should be more controlled
5 month head should be supported (head up)
Head control before standing
Gross motor before Fine motor
Birth to 5mon weight gain 5-7 lbs every week
By 6 mon weight should be doubled (14 lbs by 6
mon)
By 1 yr weight should be tripled (21 lbs)
Baby have really fast metabolisms
Eruption (teeth coming in) at 6 mon.
By 11 mon = Fine Pincer Grasp
Peek a Boo = 8 to 10 mon
Head lag should be gone by 3 to 4 months.
Toddler = Parallel play
2 1⁄2 year old = 30 mon
3 year old= 36 mon
2 years old – 300 word vocabulary
3 years old – 900 word vocabulary
***Autism can develop as early as 18 -24 mon. Are
they pointing indicting what they want or offering
what they want giving it back or reassurance of the
object they were playing with looking back at the
parent.
Toddler give much control as much as they can its
okay if they want to put on their pants before their
shirt. Word “NO” is okay autonomy. Educate parents
to let the child makes choices for their selves. Do
not let them get overwhelmed.
Assess fontanels
–
Anterior (closes 12-18 months)
–
Posterior (closes by 2-3 months
URILRI
Tonsillitis (URI) No Codeine PO Tonsillectomy
If child is allergic to Penicillin give Erythromycin
Risk for hemorrhage s/s constant swallowing happens 5 to 10
days after discharges at home.
NO STRAW!!!
Position on side or Prone for older children for drainage
Croup (URI) Worse at night time, Barking cough,
hoarseness, Inspiratory stridor,
Treatment: Corticosteroids, Hydrate to thin mucous
Epiglottitis (URI) Droplet Precautions, HIB, Emergency, DX
by a lateral Neck Xray, Treated with antibiotics, Bacterial, Do
not open their mouth, High fever >104, Drooling, Muffled
voice, can not talk, tripod position, Inspiratory stridor, Prepare
for intubation
Bronchiolitis (LRI) AKA RSV, Contact Precautions, Early than
28wks Preterm give a preventive measure Palivizumab a
prophylaxis to boost up the immune system, injections given
monthly, HX & Assessment is how it is DX
Asthma (LRI) 2nd hand smoke, obstructive, Urban area &
Roaches/ Pollutants, Obesity, Gerd, Chronic inflammation, it is
reversible, Hyper-Responsive Lungs, Atopic dermatitis
(Eczema) & Food Allergies leads to Asthma,
Emergency Med Albuterol AKA Bronchodilator (short
acting)
Reduces Inflammation Budesonide AKA Corticosteroids
Red Zone Danger Status Asthmaticus
HX & Assessment is how it is DX
Cystic Fibrosis (LRI) Both parents have to have the gene
25% child will have the gene à Autosomal recessive disease
chromosome #7
à Thick Mucus in CF ß
Break mucus by giving fluids
**CF is not only related to Respiratory but also the
intestines.
***Meconium Ileus (blockage) is the 1st sign clinical
manifestation (they won’t past their 1st stool)
How to DX: 2 sweat tests, FTT, Genetic testing, stool test for
fat (Pancreatic insufficiency)
Male is sterile, Female difficulty w/conceiving
Due to malnutrition give HIGH protein and Calorie Diet
Fat soluble supplements (ADEK)
CPT, Postural Drainage, Breathing exercises
Stridor
Wheezing and Crackles
Read More
.png)