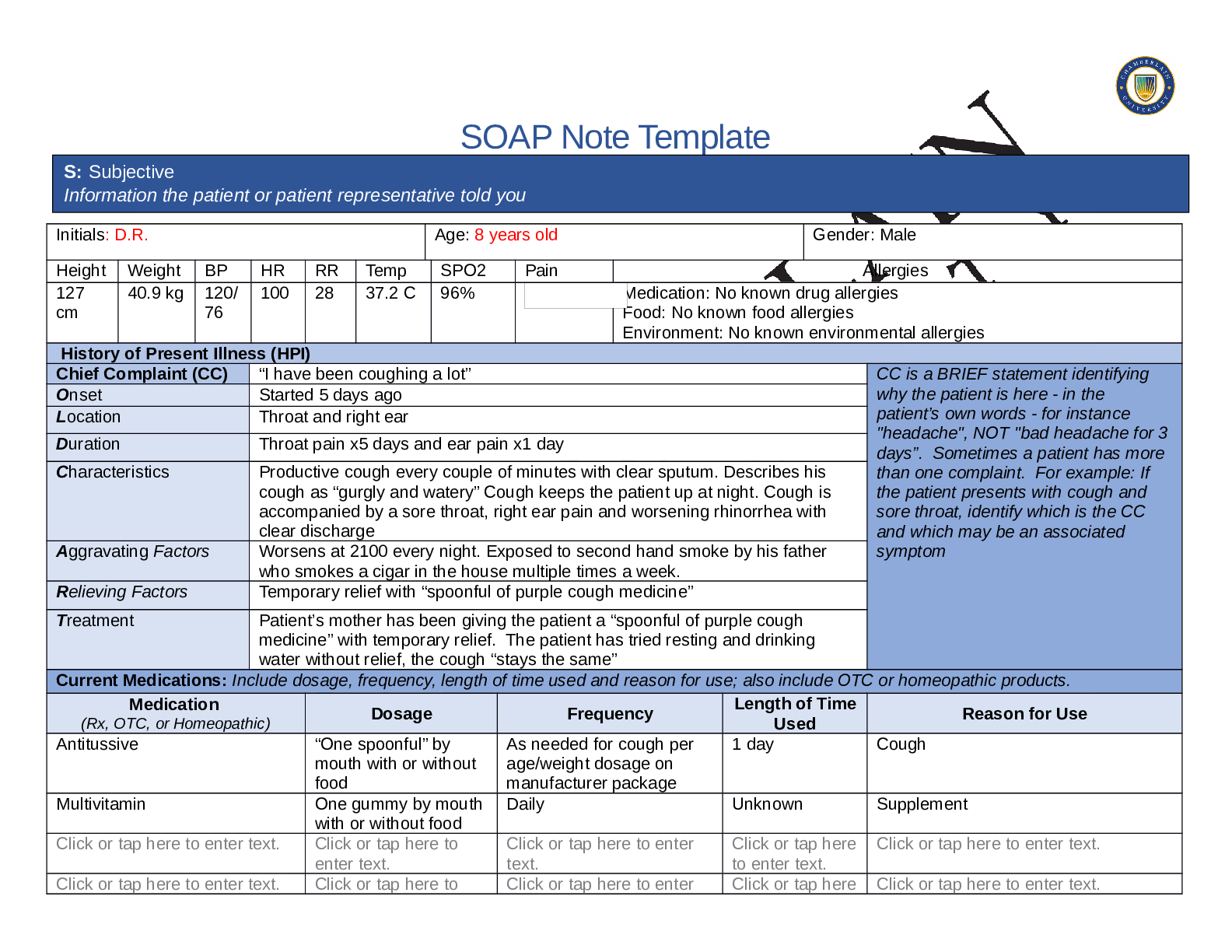
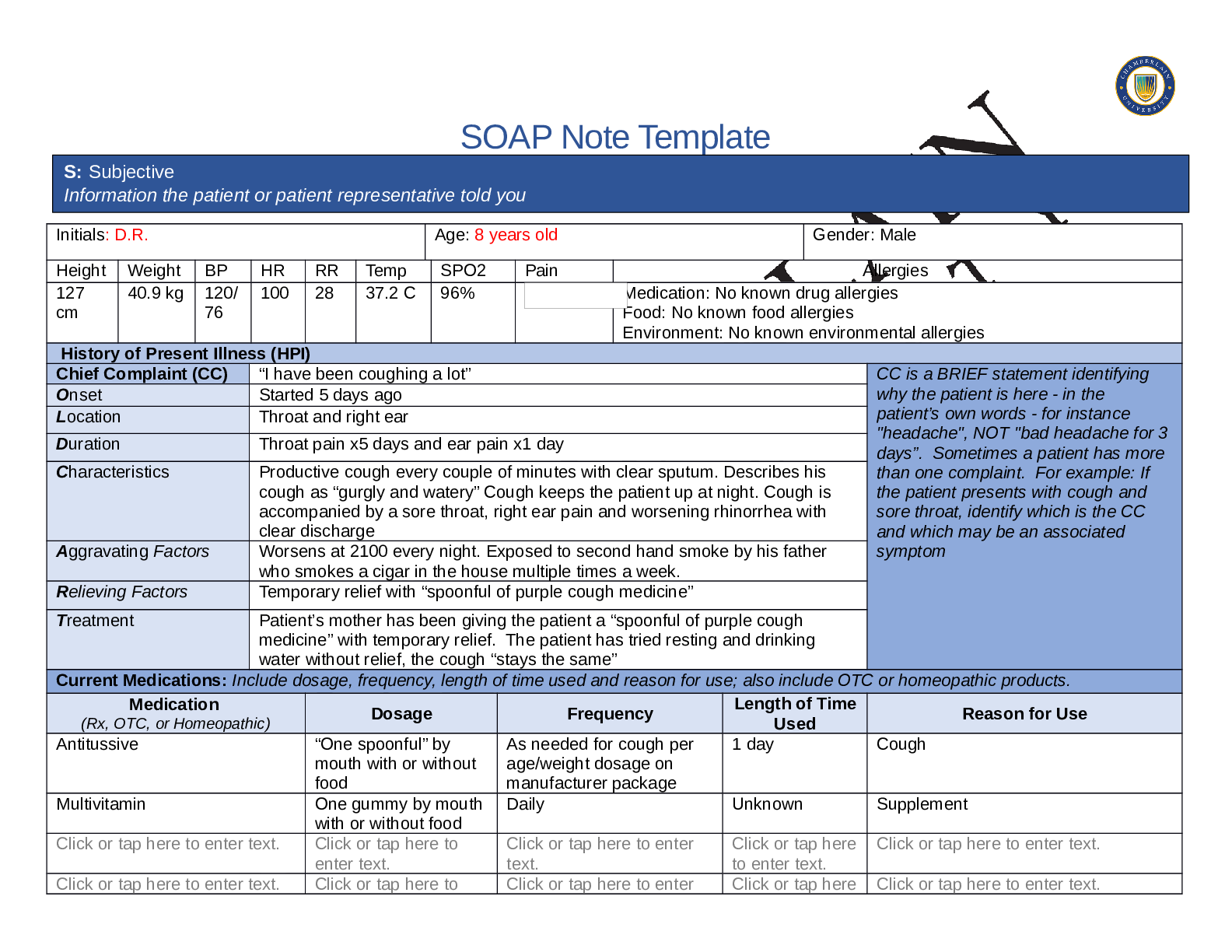
SOAP Note Template
S: Subjective
Information the patient or patient representative told you
Initials: D.R.
Age: 8 years old
Gender: Male
Height
Weight
BP
HR
RR
Temp
SPO2
Pain
Allergies
127
40.9 kg
120/
100
28
37.2 C
96%
3/10
Medication: No known drug allergies
cm
76
Food: No known food allergies
Environment: No known environmental allergies
History of Present Illness (HPI)
Chief Complaint (CC)
“I have been coughing a lot”
CC is a BRIEF statement identifying
Onset
Started 5 days ago
why the patient is here - in the
Location
Throat and right ear
patient’s own words - for instance
"headache", NOT "bad headache for 3
Duration
Throat pain x5 days and ear pain x1 day
days”. Sometimes a patient has more
Characteristics
Productive cough every couple of minutes with clear sputum. Describes his
than one complaint. For example: If
cough as “gurgly and watery” Cough keeps the patient up at night. Cough is
the patient presents with cough and
accompanied by a sore throat, right ear pain and worsening rhinorrhea with
sore throat, identify which is the CC
clear discharge
and which may be an associated
Aggravating Factors
Worsens at 2100 every night. Exposed to second hand smoke by his father
symptom
who smokes a cigar in the house multiple times a week.
Relieving Factors
Temporary relief with “spoonful of purple cough medicine”
Treatment
Patient’s mother has been giving the patient a “spoonful of purple cough
medicine” with temporary relief. The patient has tried resting and drinking
water without relief, the cough “stays the same”
Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products.
Medication
Length of Time
Dosage
Frequency
Reason for Use
(Rx, OTC, or Homeopathic)
Used
Antitussive
“One spoonful” by
As needed for cough per
1 day
Cough
mouth with or without
age/weight dosage on
food
manufacturer package
Multivitamin
One gummy by mouth Daily
Unknown
Supplement
with or without food
Click or tap here to enter text.
Click or tap here to
Click or tap here to enter
Click or tap here Click or tap here to enter text.
enter text.
text.
to enter text.
Click or tap here to enter text.
Click or tap here to
Click or tap here to enter
Click or tap here Click or tap here to enter text.
Click or tap here to enter text.
enter text.
Click or tap here to
enter text.
text.
Click or tap here to enter
text.
to enter text.
Click or tap here
to enter text.
Click or tap here to enter text.
Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses,
hospitalizations, and surgeries. Depending on the CC, more info may be needed.
Diagnosed and treated with antibiotic therapy for pneumonia last year by an urgent care clinic. At the age of 2 the patient had “a lot” of recurrent
ear infections. Patient takes a daily gummy multivitamin but when his mom is not looking he “sneaks a few extra.”
Denies surgical history, broken bones, or recent hospitilizations. Denies ear surgery or ear tubes.
Immunizations up to date with the exception of the influenza vaccine. Immunizations: Hepatitis A:2 dose series completed at 15 months, Hepatitis
B: 3-dose series completed at 6 months, Pneumococcal: 4-dose series completed at 15 months, DTaP: 5-dose series completed at age 6, MMR: 2-
dose series completed at 6 years, Polio: 4-dose series completed at 6 years old.
The patient’s mother takes him to regular doctors appointments where he receives his vaccinations.
Had epistaxis once when the patient got hit on the nose by a ball during recess.
Patient was sick a couple of months ago with an upset stomach that resolved on it’s own “pretty fast.”
Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent
data. Include health promotion such as use seat belts all the time or working smoke detectors in the house.
Third grade student in Ms. Saint-Jean’s class who likes school but bores easily when the homework is too easy. Lives with his mom (who is a
stenographer), dad, Abuelo (maternal grandfather), Abuela (maternal grandmother) and no siblings. Primarily English speaking household with
some Spanish spoken intermittently. The patient likes to play video games, read, write stories, rides his skateboard and plays with his friend Tony.
The patient wears a helmet each time he rides his skateboard. There are no pets at home. The patients father smokes cigars in the home a couple
times a week. The mother asks the father to move outside with his cigar. Reports drinking plenty of water a day due to his Abuela (maternal
grandmother) making sure he drinks enough water. Uses seatbelts consistently and has working smoke detectors in his home. Patient missed 2
weeks of school last year when he was diagnosed with pneumonia.
Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for
death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if
pertinent.
Mother-Type 2 diabetic, HTN, Hypercholesterolemia, spinal stenosis and obesity. Father-HTN, Hypercholesterolemia, childhood asthma and is a
cigar smoker in the house.
Maternal grandmother (living)-Type 2 diabetic, HTN. Maternal grandfather-Smoker and eczema.
Paternal grandmother-Died in a car accident when the patient was very young. Paternal grandfather-No known history
Read More